Health Beyond - Report of the Advisory Council on Deep-Space Healthcare
On this page
- Dedication
- Executive Summary
- Foreword
- Acknowledgements
- Chapter 1 Grasping the Torch
- Chapter 2 Launching the Vision
- Chapter 3 Scanning the Environment
- Chapter 4 Shaping the Program
- Chapter 5 Building the Team
- Chapter 6 Mobilizing the Nation
- References
- Glossary
- Acronyms and Abbreviations
- Appendix A Human Exploration Plans for Deep Space
- Appendix B Clinical, Biomedical and Performance Needs of Deep-Space Missions
- Appendix C Terms of Reference – Advisory Council on Deep-Space Healthcare
- Appendix D Advisory Council Member Biographies
- Appendix E The Expert Group on the Potential Canadian Healthcare and Biomedical Roles for Deep-Space Human Spaceflight
- Appendix F Briefings to the Advisory Council by Subject-Matter Experts
- Appendix G Candidate Members of a Canadian Deep-Space Healthcare Partnership
- Appendix H Transferring Medical Technologies Across Remote Environments
For more information on the contents of this report, please complete the CSA's Information request form: www.asc-csa.gc.ca/eng/forms/information-request.asp
For more information on reproducing the materials in this report, please contact pitt-iptt@asc-csa.gc.ca.
© Her Majesty the Queen in Right of Canada,
as represented by the Minister of Innovation, Science and Industry, .
ISBN: 978-0-660-39647-7
Margaret Nazon
Images of marvellous beadworks by artist Margaret Nazon are featured throughout our report. Margaret is a gifted beader from the Gwich'in First Nation in the Northwest Territories. The small community where Margaret lives, Tsiigehtchic, is located south of Inuvik on the Mackenzie River, beneath the shimmering auroras that dance across the Arctic sky.
Margaret is an innovator. She has re-imagined an Indigenous craft that she learned as a child to express her fascination with space exploration. By adapting traditional beading and sewing techniques in new ways, she brilliantly depicts galaxies and nebulae in vibrant colours and textures. Imagery from the renowned Hubble Space Telescope is a favourite subject.
Each beadwork is an intricate creation, requiring the stitching of thousands of glass beads of various sizes, origins and colours onto black velvet or canvas. Margaret occasionally includes bits of shell, bone, antler and driftwood. Some of her works are so layered that they become three-dimensional. The beading process is precise and exacting, but the result is lush and alluring—heavenly bodies from millions of light-years away rendered in a relatable manner.
Margaret's melding of art and astronomy is novel and perfectly aligned with the exploratory and visionary themes of our report. We are privileged that she is sharing these images with our readers.
To learn more about Margaret and her work, please visit her website at www.margaretnazon.com.
Ms. Lisa Campbell
President of the Canadian Space Agency
St-Hubert, QC
Dear President Campbell,
The Advisory Council on Deep-Space Healthcare has been pleased to deliberate on a potential new role for Canada in deep-space healthcare. Our report to you follows. It represents the culmination of months-long inquiry and collaborations among members of the Advisory Council, as well as consultations with key experts.
It was a privilege to work on a matter of such importance. Indeed, on each occasion that the Advisory Council met, our members sensed that we were engaged in an exercise of nation-building. An Agency partnership with aligned healthcare innovators could advance our national space program and benefit underserved communities. We hope the thoughts presented in our report, as well as those of the predecessor Expert Group task force, provide the ideas, clarity and guidance you seek.
The Advisory Council now wishes you and your Agency colleagues the best as you consider our recommendations. Count on us for continued support. We will always be ready to advocate on behalf of the Agency and healthcare improvement.
- Robert Thirsk (Chair)
- Diane Côté
- Valérie Gideon
- Rick Glazier
- Jas Jaaj
- Deepak Kaura
- Keith MacLellan
- Paul McBeth
- Alex Mihailidis
- David Saint-Jacques
- Terry Taddeo
- Gail Turner
- With support from:
- Gilles Leclerc
- Mary Preville
- Robert Riddell
Dedication
This report is dedicated to the memory of Dr. Arthur Maxwell House, OC, ONL (-), telemedicine pioneer and exemplary human being.
Dr. Max House obtained his medical degree from Dalhousie University Medical School in . He completed residency training at the Montreal Neurological Institute in , returned to Newfoundland and Labrador in and for several years was the province's only neurologist. He helped establish the Memorial University Medical School and served as Lieutenant Governor of Newfoundland and Labrador from to .
As a practitioner, Dr. House noted the long treks that patients living in isolated settlements throughout the province had to undergo to see a specialist. Travelling over rugged land in harsh weather conditions to seek medical care was a hardship that exacerbated the suffering from an illness. He felt there must be a better way to deliver services to rural and remote residents.
In , Dr. House launched Memorial University's telemedicine program. At first it utilized analog telephone lines. With the launch of Canada's Hermes satellite, and its successor Anik B, Dr. House began to perform medical consultations and diagnoses via satellite telephone. Video connections allowed the transmission of x-rays, brain scans and other diagnostics.
In recent decades, the telemedicine program started by Dr. House has grown and evolved. Its success is founded on his insistence that telemedicine is a network of people, not just technology. The system now links 128 telehealth sites across the province, including offshore drill ships and the Hibernia platform.
Dr. House is recognized in Canada—and globally—as the father of telemedicine. His bold vision and spirit of innovation have provided today's remote physicians, nurses and students with access to tele-education, tele-mentoring and tele-simulation resources. His advancements in telehealth services have become essential elements of healthcare delivery for patients living in remote locations around the world.
Executive Summary
The Advisory Council on Deep-Space Healthcare (the Advisory Council or Council) was established in , with a mandate to provide the Canadian Space Agency (CSA) with detailed recommendations on the scope and implementation of a national program in deep-space healthcare. Furthermore, we were to identify which Canadian organizations could be suitable partners of a CSA-led collaboration that would position Canada internationally at the crossroads of spaceflight and terrestrial healthcare innovation.
Our overriding recommendation is for the Canadian Space Agency to advance deep-space healthcare as a new strategic Agency priority. This would require investing ample budgetary and operationally oriented human resources for a major clinical program that would advance national capability and credibility in remote healthcare. It would position Canada in a critical international role in deep-space exploration. To this end, the CSA, in coordination with founding partners, would need to immediately develop a Roadmap for Action that translates recommendations from the Advisory Council, and the antecedent Expert Group on the Potential Canadian Healthcare and Biomedical Roles for Deep-Space Human Spaceflight, into action programs leading to two goals:
- For the federal government to designate deep-space healthcare as Canada's next exploration priority (an urgent near-term goal).
- For NASA to assign Canada a major leadership role in deep-space healthcare (a medium-term goal) as a means to enhance crew well-being and performance, and to reduce mission risk.
To this end, the Advisory Council makes eight recommendations that would establish deep-space healthcare as a driver and exemplar program of a national collaboration in remote healthcare innovation.
- Recommendation 1
-
Elevate deep-space healthcare to a strategic priority at the Canadian Space Agency.
- Recommendation 2
-
Pursue with determination an eventual Canadian leadership role in astronaut healthcare, well-being and performance for deep-space missions, starting with major contributions to the Lunar Gateway and Artemis programs.
- Recommendation 3
-
Leverage the vision for human space exploration and deep-space healthcare solutions by transforming healthcare delivery for medically underserved populations.
- Recommendation 4
-
Build on Canada's unique model of competency- and team-based medical education and its industrial leadership in simulator-based training. Pursue a deep-space leadership role in the development of advanced training and simulation approaches to build, maintain, credential and certify the skills of crew medical officers.
- Recommendation 5
-
Establish a Northern Demonstration Site Program as a means to test and evaluate remote clinical approaches and innovations, and to nurture fruitful relations with Indigenous communities and other critical stakeholders.
- Recommendation 6
-
Leverage the combined expertise and capacity of Canada's research and innovation communities and the health and biomedical technology sector to accelerate the development of solutions for deep-space healthcare challenges.
- Recommendation 7
-
Exploit Canada's expertise and capacity in artificial intelligence to develop remote healthcare solutions in space and on Earth.
- Recommendation 8
-
Develop a Canadian public outreach strategy and cultural exchange focused on remote healthcare in space and on Earth.
As a group, these recommendations represent a "stretch
" for Canada—the ultimate test of their validity—and a program that would be nationally critical, visible, scalable, affordable and socially beneficial.
The Advisory Council deliberated on the nature of a CSA-led national partnership. As the investments and challenges of deep-space healthcare will be significant, each partner would need to be committed to the long-term vision and contribute expertise and other resources, while also sharing risks.
The Advisory Council proposes a small group of founding partners spanning several healthcare sectors—government departments, health delivery agencies, frontline healthcare practitioners, research institutions and industry. These would be aligned, nationally influential organizations able to immediately engage on the near-term goal.
We then foresee a phased, stepwise growth of the partnership. Following government approval of deep-space healthcare as a priority program, membership of the partnership would expand to well-resourced organizations. In addition to the aforementioned sectors, members would come from user communities (astronauts, Indigenous peoples) and international spacefaring partners. The resulting alliance could address issues of healthcare equity, accessibility and outcomes in underserved communities, while advancing Canada's reputation as a deep-space healthcare leader.
Reflecting on the corporate identity for this national endeavour, the Council proposes the following vision statement:
By , Canada will become the regarded leader in remote healthcare delivery in space and to underserved populations on Earth.
As the mission of the program, we propose:
To assemble solutions for autonomous and technology-enhanced access to local healthcare for the benefit of people in space and on Earth.
We will support the development of healthcare delivery solutions by:
- Engaging spacefaring partners
- Engaging the Canadian healthcare user and delivery communities
- Enabling research and development opportunities
We suggest the following set of core values:
- Focus on Frontline Healthcare in Space and on Earth
- Excellence in Delivery
- Equity and Spirit of Collaboration
- Creating Economic Value
- Inspiring a Nation
The Advisory Council believes the ambitious propositions herein, championed by a formidable national partnership, could advance our space program while invigorating, modernizing and greatly improving access to our national healthcare system.
Foreword
Health Beyond: Galactic Aspiration, Earthly Innovation
Dear Fellow Earthling,
Reading government reports can be a bit like swimming in wet concrete. Fortunately, this report, published under the auspices of the Canadian Space Agency (CSA), is a notable exception.
Written by a distinguished and diverse team of volunteers who served as the CSA's Advisory Council on Deep-Space Healthcare, Health Beyond presents a visionary and exciting plan for Canada to pursue a world-leading role in designing and delivering healthcare, in the context of interplanetary exploration. Far from being an otherworldly project of limited earthly relevance, the Advisory Council has grounded its plan in various of the challenges facing healthcare in this country of vast distances, thinly populated expanses, rugged geography and climatic extremes.
The good news is that Canadian entrepreneurs, scientists and professionals have long been outstanding healthcare innovators, not least in remote delivery of care. The bad news is that Canada's healthcare ecosystem has struggled at times to create the collaborative networks needed to develop great ideas into scalable innovations, and to demonstrate the value of the resulting products and services. Therein lies the magic of the Advisory Council's vision. It is hard to imagine better inspiration for multi-sectoral and pan-Canadian healthcare collaboration than internationally commissioned projects tied to interplanetary travel. Nor could any context be more exacting than deep-space healthcare to prove the worth of made-in-Canada innovations.
Before going further, however, let's deal first with the elephant in the room: The world is a mess. Why should we be keen on deep-space travel now? Those sentiments, alas, have grounded our species for decades. A reminder: The first human landing on the Moon took place 52 years ago, in , and the last time we walked on the Moon was in . Space programs continued with an exciting agenda of research, discovery and international collaboration, built around a series of orbiting space stations. But does anyone still believe that our species gained something from mothballing deep-space exploration projects that might draw together our best and brightest to tackle unthinkable challenges? Is it just possible that our sense of shared humanity and collective commitment to address burning global issues might be affirmed if all on Earth could look to the skies and know that people from diverse backgrounds were en route to other planets as representatives of homo sapiens? For that matter, are we really going to abandon space travel to thrill-seeking billionaires and tourists seeking brief relief from the gravity of this world's problems?
In reality, necessity is the mother of invention, and invention in turn becomes the mother of necessity in the virtuous cycle that defines positively disruptive innovation. Multiple healthcare systems worldwide have embraced virtual care as never before during the global COVID-19 pandemic. Although appalling inequities in vaccine access persist across nations, the crisis galvanized unprecedented speed and international collaboration in developing vaccines and testing treatments for SARS-CoV-2. In like fashion, a host of innovations highly relevant to care-at-a-distance would emerge from planning for the range of medical emergencies that could occur in the course of a multi-year interplanetary journey.
Excuse me. Did you just say that Canada has no business being involved in deep-space exploration? Here, too, some reminders are in order. Canada was an early leader in aeronautical engineering, and in the late 1950s was moving fast with plans to produce both the world's first commercial jetliner and its fastest jet combat aircraft. When the Avro Arrow was cancelled in , NASA swept in days later and interviewed more than 50 Canadian scientists and engineers. By early April, 32 Canadians had already joined the U.S. Space Task Group. Many were pivotal in the Apollo 11 mission that first put a human on the lunar surface. Canada also contributed the lunar module's landing legs and an innovative antenna to Apollo 11.
Over the past four decades, Canadian astronauts have been key contributors to work involving the space shuttle and the International Space Station (ISS). Two Advisory Council members—Robert Thirsk (Council chair) and David Saint-Jacques—are physician-astronauts who each spent over six months on the ISS. In , Canada was the first country to commit to NASA's Gateway space-station project, and the renowned Canadarm continues to be an essential robotic tool for use in space, with an AI-powered Canadarm3 currently under development. Indeed, not only is Canada the longest-standing and closest national partner of NASA, the CSA also has a deepening partnership with the European Space Agency. This ability to broker and partner widely is an essential part of Canada's advantage in international projects. As to the remote healthcare connection, this too makes sense for the country where telemedicine was pioneered, where innovative robotics in space is already a national tradition, where the foundations of the global AI revolution were laid, and where for decades the pace and quality of medical and healthcare research has outstripped peer nations of similar size.
In short, the Health Beyond report strikes many positive chords with its call for inclusive and fearless innovation, its emphasis on multi-sectoral and multi-stakeholder partnerships, its assertion of the enduring value of national and international collaboration, its pragmatic focus on ways to capitalize on our national assets and our environment, and its confident belief that technologies developed for deep space can be deployed right here in remote and underserved parts of Canada, providing both healthcare and economic benefits to our nation in the process.
Last and not least, the soaring ambitions of Health Beyond should be celebrated as Canada begins to rebuild in the wake of the most serious public-health crisis to hit our nation in more than a century. There is clearly much work to be done to create a better Canada, but every reason for us to imagine a future for our country in which the sky is no longer the limit.
Happy reading!
Yours sincerely,
C. David Naylor, OC, MD
Acknowledgements
Much like the work of an astronaut crew, the work of a task force is dependent on the commitment and skills of a large team of talented individuals. We acknowledge this indispensable support and wish to express our gratitude to many people who toiled unassumingly but reliably behind the scenes.
First and foremost, we give credit to a remarkable group of individuals from the Canadian Space Agency and Indigenous Services Canada who were matrixed into a "super secretariat
" known as the Health Beyond team. The Advisory Council couldn't have fulfilled its mandate without their operational and administrative support. Throughout our mandate, the team coordinated upcoming meetings and workshops, followed up on action items, conducted research and analysis, drafted this report and provided updates to Council members between meetings and workshops.
The Advisory Council wishes to specifically thank the following Health Beyond team members for their time, expertise and enthusiasm: Isabelle Tremblay, Patrick Sullivan, Robert Riddell, Nicole Buckley, Jean-Marc Comtois, Raffi Kuyumjian, Linda Dao, Maja Djukic, Sally Rideout, Nada Fadol, Annie Martin, Bradley Andrews, Perry Johnson-Green, Bruno Hardy-Chartrand, Sebastien Lafrance, Alain Ouellet, Charlotte Pearce, Matthew Bamsey, Christian Lange and Anastasiia Prysyazhnyuk of the CSA, as well as Barbara Guy of Indigenous Services Canada.
We especially thank Maja Djukic and Sally Rideout, who served as executive secretaries to the Advisory Council, our go-to persons whenever we encountered a problem. Admiration and special gratitude are directed to Sally Rideout, who planned and facilitated the Advisory Council brainstorming workshops. Sally has a knack for eliciting rich discussions and achieving consensus in a diverse group of opinionated individuals on topics ranging from vision, mission and values to elevator pitches and ideal partner attributes. Each of her workshops was enjoyable and productive.
Secondly, we thank several esteemed national experts who generously shared their thoughts on a variety of leading-edge topics in space, health, innovation and research: Evan Adams of the First Nations Health Authority; James Rourke and Stu Iglesias of the Society of Rural Physicians of Canada; Anna Goldenberg of the Hospital for Sick Children and the Canadian Institute for Advanced Research; Garnette Sutherland of Project neuroArm at the University of Calgary; Mehran Anvari of the Centre for Surgical Invention & Innovation at McMaster University; Jas Jaaj, Joyce Drohan and Niraj Dalmia of Deloitte Canada; Gail Turner, formerly of the Nunatsiavut Government; Andrew Padmos, formerly of the Royal College of Physicians and Surgeons of Canada; Diane Côté of MEDTEQ+; Rekha Ranganathan of CAE Healthcare; Elissa Strome of the Canadian Institute for Advanced Research; Andrea Reed and Nicole Robinson of the Canadian Partnership Against Cancer; Deepak Kaura of 1Qbit; and Terry Taddeo and Sharmi Watkins of NASA Johnson Space Center. Their briefings were foundational to our deliberations, served to bring all members up to a common level of understanding and helped shape the content of our final report.
Thirdly, we thank the senior leadership of the Canadian Space Agency for the invitation to Advisory Council members to serve Canada. It was a privilege to come together and reflect on such a compelling vision for our nation. In particular, we thank former CSA president Sylvain Laporte and current president Lisa Campbell for their encouragement. We also thank Gilles Leclerc, Director General, Space Exploration, and Mary Preville, Vice-President of Space Program Policy, for their wise counsel. This level of support well demonstrated to Advisory Council members that the CSA has the leadership and governance practices to oversee a national partnership.
We are grateful for the support of Dr. David Naylor, OC, in our endeavour, and honoured that he has written the foreword for our report.
We are privileged that artist Margaret Nazon has shared imagery of her remarkable beadwork to help tell the story of space exploration. Margaret's ability to figuratively bring the heavens down to Earth is an apt metaphor for the potential of deep-space healthcare to bring benefits to remote and underserved populations.
Finally, we thank our writer, Mary Gooderham, whose astute edits of our report made us look more concise than we really are.
While recognizing the contribution of the aforementioned individuals, members of the Advisory Council emphasize that we alone are accountable for what we present in our report.
Chapter 1 - Grasping the Torch
In this section
"But you, brave and adept from this day on … there's hope that you will reach your goal … the journey that stirs you now is not far off."
Background
Global Space Exploration Plans
There is a growing and shared desire among spacefaring nations to venture beyond low-Earth orbit in the coming years. Accordingly, a group of 26 international space agencies, led by NASA and including the Canadian Space Agency, has collaborated over the last decade to develop a notional plan to explore deeper into the solar system. Known as the International Space Exploration Coordination Group, it has published a plan—the Global Exploration Roadmap and a Roadmap Supplement—describing how a sequence of human and robotic deep-space missions could unfold in the coming years. An overview of this roadmap is provided in Appendix A – Human Exploration Plans for Deep Space.
The term deep space is used by the group to describe possible missions in the inner solar system, with intriguing destinations such as lunar orbit, the surface of the Moon, a near-Earth asteroid and Mars. A human mission to the surface of Mars, projected to launch in the mid-2030s, is its primary goal and ultimate objective. A voyage to the red planet will help answer some fundamental questions:
- What can the geology of Mars teach us about Earth's past, present and future?
- Was Mars ever home to life?
- What can Mars teach us about the start of life on Earth?
- Could Mars one day be a safe second home for humans?
Operational and Technical Challenges of Deep-Space Missions
The next few years of human spaceflight will focus on construction of the Lunar Gateway, a mini space station in lunar orbit, and on utilizing a research base at the south pole of the Moon. Planning for human exploration missions to the red planet will then ensue. This will be an ambitious undertaking, with many challenges. It will require a decade-long commitment and a concerted effort by several nations to land an astronaut crew on Mars and return them safely.
Some challenges of this new class of deep-space missions will be operational. A flight to Mars, for instance, will feature:
- Long distances (200 million kilometres) and duration (two-and-a-half years)
- Limited crew size
- Limited volume, mass and power allowances of onboard equipment and systems
- Minimal or no cargo resupply
- Communication latencies (six to 20 minutes one-way) resulting in reduced ability of Mission Control to assist the astronaut crew with urgent and inevitable mission contingencies that arise.
Other challenges are technical. A report by the U.S. National Research Council identifies 10 essential technologies that must mature before a crewed Mars landing mission is feasible. All vehicle systems will need to be more reliable and robust than those of spacecraft that do not venture as far from Earth. All must function autonomously, with limited monitoring and control by flight-controllers on the ground. Life-support systems will need to be closed loop design.
Crew Health, Well-Being and Performance Issues of Deep-Space Missions
Delivery of healthcare to future astronauts may be the most significant challenge of deep-space exploration. Venturing beyond Earth's orbit will expose astronauts to harsh environmental conditions and novel risks. These, if unmitigated, would jeopardize the health, well-being and performance of the crew.
In past missions, the concept of medical operations has been Earth-centric. The health of astronauts aboard the International Space Station (ISS) and other spacecraft in low-Earth orbit has been managed by a medical team on the ground. This concept of medical operations was made possible by the availability of real-time data and voice communication with the crew, and with a medical-evacuation option if necessary.
This will become impractical once astronauts venture to deep space. Ground-based oversight in urgent situations will not be possible. Medical evacuation of a seriously ill or injured crew member to Earth will no longer be an option. The onboard medical facility, limited in size, will need to support complete and autonomous care for health and cover all medical and surgical eventualities.
Venturing to deep space means we must rethink the operational approaches, crew training and critical technologies relied upon to manage astronaut health. The delivery of healthcare must become independent of Earth. Autonomous and semi-autonomous concepts must be developed and validated. Before the first crew launches, medical care must become more patient-centric, point-of-care and virtual.
Detailed operational considerations for the delivery of healthcare to deep-space astronaut crews are provided in Appendix B – Clinical, Biomedical and Performance Needs of Deep-Space Missions.
Canadian Space Exploration Plans
The daunting nature of these future space missions appeals to Canada's heritage of exploration and the national spirit of innovation—an opportunity to measure the best of energies and skills.
A focus on deep-space exploration underpins Canada's strategic plan Exploration, Imagination, Innovation: A New Space Strategy for Canada. It includes a commitment to participate in NASA's Lunar Gateway program, leveraging existing strengths like robotics while advancing others such as healthcare innovation.
The strategy specifically mentions a role in the health management of deep-space astronauts:
"By leveraging Canada's health and medical research expertise, and emerging technologies such as artificial intelligence, Canada will advance autonomous medical systems to support astronaut health in space and health outcomes at home. Through the Lunar Gateway project and via new efforts on Earth, Canada will explore questions key to improving healthcare and quality of life for Canadians."
Furthermore, an objective of this strategy is to ensure investments in space exploration bring practical benefits to Canadians. The CSA will work with stakeholders to translate novel approaches developed for spaceflight to improve the lives of Canadians on the ground.
The Advisory Council on Deep-Space Healthcare
Our Task
To advance the New Space Strategy healthcare vision, the CSA established a task force—our task force—in , known as the Advisory Council on Deep-Space Healthcare (the Advisory Council or Council). Our mandate was to:
"…assist the Canadian Space Agency as it endeavors to define in detail a potential deep-space healthcare program for Canada that is nationally critical, visible, scalable, affordable and socially beneficial."
In other words, the Advisory Council was to describe in practical detail how the CSA could establish a major new program addressing the crew health, well-being and performance issues of deep-space exploration. Furthermore, we were to "identify potential national partners and stakeholders with mandates and priorities aligned with those of this potential initiative,
" in order to form a CSA-led partnership that could position Canada internationally at the crossroads of spaceflight and healthcare innovation. The Terms of Reference for the Advisory Council are provided in Appendix C and biographies of our 15 members are provided in Appendix D.
Our Council builds upon the work of a predecessor task force, the Expert Group on the Potential Canadian Healthcare and Biomedical Roles for Deep-Space Human Spaceflight. Its report was well received by the CSA and national stakeholders. The work of this Group and its findings are summarized in Appendix E.
We endorse the spirit and recommendations of the Expert Group and agree a CSA-led partnership should pursue an audacious goal—a leadership role in deep-space astronaut healthcare. With this current report, the Advisory Council advances that Group's work by addressing implementation issues of its vision.
Overview of the Health Beyond Report
When the Advisory Council was launched in late , our initial conversations were largely framed around an exciting new challenge for Canada in space exploration. As our primary task, we were to consider new approaches to enable the delivery of healthcare to intrepid astronauts venturing into deep space. Spinning off space innovations to also benefit patient care on Earth was an additional and important objective to be examined.
As the work of the Council progressed and, concurrently, the COVID-19 pandemic inflicted its wrath on marginalized populations, the plight of underserved communities came into even sharper focus. Residents of remote and Indigenous communities, those in long-term care homes, and others in situations such as homelessness are clearly disadvantaged by limited access to medical services and substandard health outcomes.
Several members and invited subject-matter experts (referenced in Appendix F) encouraged the Council to more closely examine issues of healthcare access, equity and outcomes. They felt new approaches and technologies developed for spaceflight could be transformative for healthcare delivery to underserved populations.
We wholeheartedly agree. Addressing the issues of healthcare delivery to underserved populations should not be viewed as a nice-to-have spinoff of a space exploration initiative, but as an imperative. We deem the space and terrestrial challenges of equal importance; the pursuit of one is not possible without the other. Many clinical, research and commercial organizations would be eager to assist the CSA on space matters if terrestrial issues could also be addressed.
In the following chapters, a deep-space healthcare program for Canada is outlined. We describe a collaborative national alliance encompassing the space, healthcare and innovation communities that could elevate Canada's capability and standing as a world leader in deep-space exploration. This would be a synergistic collaboration in which the capability of the alliance to move both space and social yardsticks is greater than the sum of the individual members.
We have written this report so our message is clear to readers who do not have a background in spaceflight, healthcare or innovation. Nevertheless, there are several specialized terms that may be unfamiliar. We include definitions of these in the Glossary. They are identified as blue hyperlinks. Clicking on the term will take you to its description.
We also back up declarative statements in the body of the report with substantiating references. Source publications and further words of explanation can be found in the References section of this report, organized according to chapter.
Chapter 2 - Launching the Vision
"Skate to where the puck is going, not to where it is."
Vision, mission and values statements are vital elements of new initiatives and organizations. They provide high-level goals, purpose and identity to participants. They are a framework upon which a strategy can be built.
The thoughtful crafting of foundational principles was regarded by the Advisory Council as one of the more important tasks of our mandate. They can set a clear direction for a nascent partnership in deep-space healthcare and then guide the partners through the inevitable twists and turns of the ensuing journey. They provide clarity to national stakeholders that engage with the partnership.
Vision
A vision statement is a concise, aspirational assertion of the strategic direction in which an organization wishes to move. It defines the organization's long-term goal, its envisioned destination. It expresses to partners what long-term success should look like.
The Advisory Council lauds the preceding Expert Group's aspiration of an enlarged role for Canada in the exploration of space. Accordingly, we propose the following vision statement for a deep-space healthcare partnership:
By , Canada will become the regarded leader in remote healthcare delivery in space and to underserved populations on Earth.
Note this statement specifies a nine-year time horizon. Rather than using the present day as a starting point, we imagine the future and work backward. This "future-back
" approach will guide the partnership as it builds toward a new reality. Quantifying the vision with a timeframe also allows the partnership a means to scope its strategic planning process and to measure progress.
Mission
A mission statement is a brief, clear and compelling statement that defines the fundamental purpose of an organization. Its activities can be justified if they are included in the mission statement. A well-crafted mission statement is informative for what it leaves out.
The mission statement proposed for the deep-space healthcare partnership includes roles for Canada in space and on Earth, as well as services that will be provided to our international partners and Canadians.
To assemble solutions for autonomous and technology-enhanced access to local healthcare for the benefit of people in space and on Earth.
We will support the development of healthcare delivery solutions by:
Engaging Spacefaring Partners
The systematic and continuous engagement of spacefaring partners will signify that Canada is taking a leadership role in deep-space healthcare and will help achieve consensus on what is required.
Engaging the Canadian Healthcare User and Delivery Communities
This includes:
- Providers (health authorities, Indigenous communities, physician practices), regulators, industry, care practitioners, provinces and territories, academia, educators, and all levels of government.
- People (patients)
Enabling Research and Development Opportunities
This includes:
- Fostering technology-development opportunities that can be translated to delivery of care in terrestrial and space settings
- Job creation, bringing Canadian economic growth
- Creating an environment for technology demonstration and clinical validation
Values
Organizational values are about identity and culture. They describe the unique character and behaviour of leaders and staff, differentiating their organization from other players in the field. When values become integrated into work processes and decision-making, there is a clear link with organizational performance.
The following principles are proposed as core values for the partnership staff and leaders:
Frontline Healthcare in Space and on Earth
Frontline healthcare practitioners and their patients are our primary focus. We will create and implement technologies that equip, train and support health teams to protect the well-being and performance of their patients in space and on Earth.
Excellence in Delivery
Operations in harsh environments are complex and risky, with little or no margin for error. We will create partnerships that relentlessly pursue excellence in healthcare delivery with dedication, preparation and vigilance.
Equity & Spirit of Collaboration
Inherent to Canadian values, supporting the provision of equitable and pervasive healthcare will be a defining feature of our work. We recognize this program will ultimately provide health services to Canadians and the international community. Perspectives and contributions from our partners are therefore paramount. We will ensure the systems we implement operate across a representative population and help address national challenges in remote healthcare accessibility and equity.
Creating Economic Value
Combining space and healthcare partners in a joint venture will provide a unique opportunity to connect, engage and inspire technological innovation. This will showcase capabilities in space and healthcare delivery to create new economic opportunities for Canadian industry. By leading in deep-space healthcare, Canadians will be emboldened to think differently.
Inspiring a Nation
The possibility and potential to create substantial change for such a grand challenge as healthcare will ignite creativity and passion to think big and be bold. It will inspire youth to pursue STEM (Science, Technology, Engineering, Mathematics) and healthcare careers, adding further value to the cultural and economic foundation of Canada.
Chapter 3 - Scanning the Environment
In this section
"Know Thyself"
New organizations do not operate in a vacuum. There are a number of external influences and internal forces that shape their ambitions and affect their operations. A SWOT (strengths, weaknesses, opportunities, and threats) framework is a useful management tool to help identify and organize these factors. A SWOT analysis is often employed by organizations as a first step in the strategy-development process.
The Advisory Council conducted a SWOT analysis to determine the relevant factors that would support or impede a deep-space healthcare initiative. We began by assessing the space, healthcare and innovation environments in which the initiative would function. Our analysis identified five opportunities that support the ambitions of a healthcare partnership, as well as two threats.
Opportunities
A Yearning to Venture Beyond Low-Earth Orbit
The last Apollo astronauts departed the Moon a half-century ago. Since then, human space missions have been confined to low-Earth orbit. However, mounting international interest in exploration, embodied in the International Space Exploration Coordination Group, has now inspired concrete plans to jointly venture farther in space and to undertake more ambitious missions.
The global impetus behind space exploration is evidenced by rising investment. Annual budgets for exploration programs of international space agencies rose to $20 billion in , and are expected to reach $30 billion a year in the next decade. While most of this investment comes from major players such as the U.S., China and Europe, new players like India, South Korea and the United Arab Emirates are also investing and planning bold missions. Large, collaborative international programs are particularly attractive, representing a means for national space agencies to extend their political influence, foster knowledge-creation and enable technology transfer.
The scope of future exploratory missions has expanded to include roles for private companies. The exponential growth of the commercial space economy, driven by new capabilities and disruptive innovations, has led to sustainable business models and the opportunity to collaborate with government space agencies.
Addressing Access and Medical Outcomes for Remote and Underserved Populations
One fifth of Canadians live in non-urban areas. Our relatively large remote population and sparsely populated landscape present challenges for the delivery of accessible and equitable healthcare. These challenges also present a unique opportunity.
Physical distances and the challenges that medically isolated people face have always meant that some Canadians, such as those living in remote communities and older adults, have difficulty getting timely access to medical diagnoses and treatments and are underserved compared with other Canadians.
Innovations required to enable deep-space missions could also provide healthcare delivery solutions in our remote communities. For example, robotics-enabled healthcare, portable medical devices, health-data storage and analytics could improve the timeliness, quality and continuity of care. Telehealth, virtual and sensor technologies could augment pre-transport clinical decision-making and reduce the time that patients must spend away from their northern homes to seek tertiary care in the south.
Rapidly Changing Needs of Aging Canadians
Senior citizens make up 17% of the Canadian population and comprise the fastest-growing segment of our population. This trend will continue into the 2030s as the baby-boomers age. Canada's healthcare system is not designed to address the continuum of care/rapidly changing needs of our aging population. A national seniors' strategy and a new delivery model are needed to better manage the complexities of chronic diseases and to support the growing number of seniors who desire to age at home, as well as to support their families and caregivers.
Technology solutions for space will overlap with the telehealth needs of the aged. These include tele-monitoring of health and environmental conditions (e.g., motion sensors, wearables), AI-enabled diagnostic and predictive solutions, health and social-care robotics, and digitalization and portability of health records to facilitate patient transfers.
Healthcare Gaps Exposed by the COVID-19 Pandemic
The COVID-19 crisis exposed many gaps in the Canadian healthcare system. Our vulnerable populations were most affected by the pandemic. Travel restrictions, for instance, disrupted access to medical expertise and healthcare facilities for some Indigenous communities and chronic-care patients. The crisis also exacerbated isolation and confinement, loss of employment and reduced access to recreational activities.
Synergies exist between approaches to healthcare delivery for deep-space astronauts and strategies to mitigate COVID-19-exposed shortcomings. These include environmental monitoring and communication technologies, patient monitoring and testing systems, virtual access to medical expertise and treatment capacity. We highlight three synergistic opportunities:
Remote Care
Remote care is a solution that brings healthcare to people, rather than transporting people to care. Benefits of this model of care include timely access to treatment as well as cost-savings and culturally safe care. Advances such as environmental monitoring, improved (smaller/cheaper) technology for water treatment and virtual patient-doctor interaction tools, as well as enhanced imaging and analytical capabilities all intersect with technologies for deep-space healthcare.
Patient Empowerment
The World Health Organization defines patient empowerment as "a process through which people gain greater control over decisions and actions affecting their health.
" Within global health and social-care strategies, empowerment has become a key theme.
Recent innovations are driving the evolution of care toward more patient-centric approaches. Medically isolated populations are being supported with technology resources to make better decisions and take more action concerning their own health and well-being, similar to what will be provided to deep-space astronauts. These are powerful tools to promote medical autonomy.
Mental Health
E-health is a rapidly evolving technology directed at enhanced remote diagnosis and support for the self-management of illness. Healthcare systems are increasing their investment in such technology. Patients facing prolonged isolation and confinement will benefit from the capabilities of e-health tools specific to mental-health disorders.
Synergistic Alignment with National Priorities
National pursuit of a deep-space healthcare initiative would complement several existing social needs and economic priorities. We identify four opportunities for national collaboration:
Accelerating Innovation and Scaling up of SMEs
Federal and provincial governments have made repeated investments in digital health technologies at all stages of development, from research to adoption. These investments have spurred economic growth and created quality jobs. Examples include the Digital Technology Supercluster in BC, the National Research Council Challenge programs and the industry-led Medical Innovation Xchange.
Improving Quality of Life in Indigenous Communities
The federal government is committed to building a stronger, more inclusive and resilient nation, with a particular focus on Indigenous peoples. Distinctions-based health legislation is being co-developed with Indigenous leaders. The Arctic and Northern Policy Framework nurtures healthy families and communities, supports collaborative approaches, develops equal partnerships, and recognizes and protects Indigenous rights. Investment in high-quality healthcare will target improved access to health services, where and when they are needed.
As a signatory to the United Nations Declaration on the Rights of Indigenous Peoples, Canada acknowledges the right of Indigenous peoples to be actively involved in developing and determining health programs that affect them, as well as their right to enjoy the highest attainable standard of physical and mental health (Articles 23 and 24).
Improving Healthcare Systems and Delivery
The report of the Advisory Panel on Healthcare Innovation concluded that Canada's healthcare systems are ill-prepared to respond to contextual shifts. Many available innovations are being slowly adopted (e.g., precision medicine) and yet are not meeting needs. To enhance the quality and sustainability of Canadian healthcare, the Panel encouraged the scaling of innovations, the coordination of reforms and the seamless delivery of multi-disciplinary practitioner care across provincial jurisdictions.
Supporting Canadian Leadership in AI and Quantum Computing
Canada is globally recognized as a leader in artificial intelligence (AI) and machine learning. The country has three world-class AI institutes, the Vector Institute in Toronto, the Montreal Institute for Learning Algorithms (Mila) and the Alberta Machine Intelligence Institute (Amii) in Edmonton.
The federal government is determined to maintain Canada's international AI reputation. In the federal budget, the Pan-Canadian AI Strategy was bolstered by an additional investment of $444 million over 10 years. CIFAR and the AI Institutes have established the advancement of healthcare research, training and innovation as a strategic priority in the next phase of the Strategy. Leveraging Canada's AI research ecosystem and population-wide health data holdings will enable the development and adoption of many AI-enabled health applications and underpin the development of new diagnostic tools and treatments. It will foster improvements in health service delivery and provide insights into both disease prevention and population health policy.
Addressing Climate Change
Global climate change is one of humanity's most pressing issues. It represents the greatest health challenge of our time, threatening to disrupt many aspects of society and the long-term survival of humankind. The physical and social impacts of global warming are widely recognized; current research suggests we are approaching the point where it may be irreversible. Many of our ecosystems are unable to adapt to the current pace of climate change. Canada is not immune. The country is warming at an alarming rate, with the most significant effects in the Canadian North. These changes disproportionately affect marginalized groups, including First Nations and Inuit populations in Canada.
Social and environmental determinants of health, including clean air, safe drinking water and food sources, and secure shelter will be directly affected by climate change. As this situation worsens, more people will face the health consequences of extreme weather events. These can disrupt almost every aspect of daily life, including transportation infrastructure, healthcare systems and communications networks. Such systems are critical to maintaining access to emergency services and healthcare.
In , the federal government introduced its climate plan A Healthy Environment and a Healthy Economy. The plan is designed to reduce greenhouse gas emissions and achieve Canada's Paris Agreement target. It builds on the actions of the Pan-Canadian Framework on Clean Growth and Climate Change. Health Canada is leading the development of the Health of Canadians in a Changing Climate: Advancing our Knowledge for Action report, with a planned release later this year. This report will assess the risks of climate change on the health of Canadians and to the health care system. It is intended to support future decisions and actions by health officials at local, provincial/territorial and national levels.
Threats
Competition for Meaningful Roles in Deep-Space Healthcare
Other spacefaring nations have already indicated their intention to pursue the near-term leadership role in deep-space healthcare. This would become a valued niche area of national competence for any space agency. No country currently has experience or capability in the field, so securing the first-mover position is strategic and will be associated with advancements in technology, economic benefits and new jobs.
NASA has developed a Medical System Concept of Operations and a Medical Data Architecture for Lunar Gateway and Artemis Phase 1 missions. The U.S. agency has invested resources to develop exploration medical capability. Similarly, the European Space Agency (ESA) has declared its intent to be a major player. ESA has shared a medical system concept for the International Habitation Module (iHAB) of the Lunar Gateway station, featuring standard interfaces and data architecture, bio-diagnostics and countermeasure devices.
The competition is further intensified by looming deadlines of the Lunar Gateway and Artemis programs. In the upcoming months, NASA is expected to allocate healthcare roles and contributions by partners. While Canada is not prepared to play a leadership role in Lunar Gateway/Artemis, it will be strategic and urgent to secure a meaningful contribution and sub-system responsibility, as a means to position our country favourably for longer-term ambitions.
A Challenging Domestic Market for Healthcare Innovation
The Advisory Panel on Healthcare Innovation in its report found that entrepreneurs across Canada have difficulty introducing, sustaining and scaling up innovations in the healthcare system, given system fragmentation, a risk-averse culture and an inadequate focus on understanding and optimizing innovation. A deep-space/remote healthcare partnership would need to identify ways to enable the transition of health innovations from idea to market, with notable attention given to raising capital and successfully navigating regulatory approvals.
1. Complex Regulatory Environment
The regulatory environment in the Canadian health and biosciences sector is complex. It presents challenges to innovators, who must navigate the labyrinthine system of regulatory approval. The resources of small businesses can be quickly depleted by drawn-out processes.
It also hampers the ability of Canadian companies to participate in larger global markets, as securing approvals for health innovations in international jurisdictions is often contingent on regulatory and reimbursement approvals in the country of origin. Digital standards and privacy regulations vary across provincial and territorial borders. The lack of a harmonized data governance framework poses a further barrier to small businesses wishing to gain access to repositories of healthcare data.
2. Limited Capacity to Commercialize
While Canada's medical device industry is well-established, it lags behind other countries in the commercialization of its innovations—the so-called "valley of death
". Proof-of-concept processes are expensive, development cycles are long and our domestic market is small. Access to key national testbeds—hospitals and healthcare providers—that could expedite commercialization is limited. Slower uptake of digital-health innovations further impedes the growth of domestic industrial capabilities.
3. Access to Canadian Capital
Health technology start-ups depend on private equity to succeed. But access to venture capital in Canada is limited. Private investors in other countries have a greater willingness than Canadian investors to fund digital health technologies and to assume risk.
To be commercially viable, companies must export their products and services to the U.S. market, which skews the direction of innovations away from the needs of the Canadian healthcare system. Furthermore, U.S. tax incentives for foreign investment have been expanding, drawing talent, technology and potential tax revenues away from Canada.
4. The Federal/Provincial/Territorial Landscape
While the federal government oversees compliance with the requirements of the Canada Health Act, patient care in Canada is delivered through provincial and territorial jurisdictions. Each of these 13 healthcare systems has its own legislation, priorities, provider organizations, reimbursement processes and procurement systems. This siloed system creates barriers to innovators hoping to scale up promising new technologies across the nation. Their challenge is further exacerbated by the absence of national standards and strategic priorities.
With a primary focus on the delivery of patient care, innovation within healthcare systems has a lower priority. Funding models, for instance, compensate physicians on a fee-for-service basis, with reimbursement codes based on the cost to deliver a service, not the value a service provides. Thus, there is little incentive to provide services enabling better value or innovation.
Even within the federal government, innovation and health ministries have different—sometimes conflicting—goals. Some departments focus on commercialization and market-competitiveness, while others focus on patient outcomes and the management of costs.
5. Procurement Processes
The procurement processes of healthcare systems are another barrier to the adoption of innovative technologies. Procurement decisions based on price rather than measures of value place innovative products with higher upfront costs but a stronger value proposition—such as improved outcomes and the avoidance of future costs—at a disadvantage.
The COVID-19 pandemic, however, demonstrated how quickly procurement practices can adapt when crisis conditions exist. Expedited responses during the pandemic were able to quickly deploy a multitude of innovations. This was a hopeful sign for future reforms.
Strengths
With an understanding of the national and international realities that would influence a deep-space healthcare initiative, the Advisory Council next explored the internal organizational attributes of a nascent CSA-led partnership. It is prudent for an organization to be aware of its own internal strengths and weaknesses. Both can generate insights, reveal needs and present opportunities. They can raise warnings about shortcomings to be addressed.
Six key strengths and three weaknesses would characterize a CSA-led partnership.
Canada is Highly Regarded as a Reliable Spacefaring Partner
Canada is among a handful of countries with the specialized technical and operational experience required to support human spaceflight missions. National expertise in astronaut selection and training as well as space robotics has enhanced our reputation as a capable and trusted partner in large-scale international programs. Our inclusion in the Lunar Gateway partnership has reinforced this.
Canada is also regarded as a reliable and honest broker in other settings such as the UN, G7, G20 and UNESCO. We have repeatedly delivered and managed significant contributions to several international programs.
Specialized Expertise in Several Relevant Areas
Canada is an important player in the international health and biosciences community. We are regarded as a leader in clinical diagnostics, practitioner training and simulation, as well as in emerging technologies such as AI, digital health, remote medical robotics and minimally invasive surgery.
While large enough to have a global impact, our national health ecosystem remains agile and adaptable. It includes innovation hubs, accelerators and incubators, and it is supported by a vibrant industry, governments, research institutions, technology providers, physician associations, healthcare operators and trainers.
Leadership in Medical Education and Practitioner Training
Canada's expertise in medical education is particularly esteemed. Our faculties of medicine and nursing are continually developing learning tools, methods and technologies to better meet the needs of students and professionals. McMaster University, for instance, pioneered a novel approach to medical-student education called problem-based learning. This approach has been so successful that it has been adopted by 500 higher-education institutions. More recently, our competency-based training model for medical specialists has been internationally commended.
Canada is a world leader in the training of rural generalists in multiple skill-sets (emergency medicine, surgery, anesthesia, maternity care, family medicine, trauma, ultrasound, cardiology, oncology). The Society of Rural Physicians of Canada, the College of Family Physicians of Canada and the Royal College of Physicians and Surgeons of Canada continue to upgrade learning programs to better meet the needs of remote practitioners. In addition to the provision of enhanced surgical and anesthesia skills, these colleges also recognize that professional attributes like surgical courage and the ability to thrive in situations of uncertainty are assets for rural generalists. One ideally acquires these qualities by years of contextual experience, supported through networks of specialist coaches using remote-presence technology.
Montreal-based CAE Healthcare is a world leader in simulation-based medical education. Its commercial products include surgical and imaging simulation, curriculum, centre management and highly realistic patient simulators. Some 8,000 CAE simulators are in use worldwide by medical schools, nursing schools, hospitals, defence forces and others.
Expertise in Advanced Healthcare Delivery
Canadian healthcare delivery is domestically and internationally esteemed. Canadian expertise is recognized in areas such as remote and minimally invasive surgery, psychology and cognitive sciences, clinical medicine, geriatric care, public health and health services.
Satellite-based telemedicine was pioneered in the 1970s by Dr. Max House of Newfoundland and Labrador to address the healthcare needs of people living in rural and remote communities. The delivery of virtual care in Canada today continues to evolve and advance.
The COVID-19 crisis has highlighted Canadian strengths in emerging areas like quantum computing and AI. Facilitated by streamlined approval processes, medical technology firms and federal regulators were brought together by the pandemic to address urgent societal needs. Canada was the first country, for example, to approve the use of an AI-enabled system to augment the interpretation of chest x-rays by radiologists.
Research and Academic Excellence
The performance of Canadian medical researchers is extraordinary. Clinical medicine represents the largest share of all research publications in Canada and 4.1% of the global share. Of all research fields in Canada, clinical medicine has the highest level of performance in the top-cited 1% of world publications.
In the life sciences and medicine category, the University of Toronto is ranked 13th, McGill University 29th and University of British Columbia 31st by the QS World University Rankings . Six nursing schools (Toronto, Alberta, McMaster, UBC, McGill and Calgary) are ranked in the world's top 50 nursing schools.
This combination of research excellence and expertise in advanced healthcare education elevates Canada to a distinguished position on the world stage. It is no surprise that Canadian researchers and technologists are frequently sought as collaborators in international health and biomedical undertakings.
A National Mindset Shaped by Geography, Climate and Diversity
Canada's harsh climate and expansive geography have moulded the national culture and individual character. Our sparse population distributed over rugged terrain from coast to coast to coast is reflected in a uniquely Canadian approach to the delivery of remote healthcare. Similarly, our multicultural demography imposes considerations of equity, diversity and inclusion in all national undertakings. AI-enabled healthcare solutions, for instance, are founded on a national database representative of a broad ethnicity and are therefore applicable to other diverse settings.
Weaknesses
Limited Internal Capacity to Engage Indigenous Communities
A deep-space healthcare initiative that also addresses the healthcare needs of remote Canadians would benefit greatly from the experiences, insights and contributions of Indigenous partners. Involvement of Indigenous peoples in a national space program would be significant—a major step forward in reconciliation. However, Indigenous communities must be engaged in a respectful and thoughtful manner. Indigenous peoples must define the nature and scope of their own participation and ensure that the initiative unfolds in a way that will be transformative for their participating communities.
The CSA, however, does not have a depth of expertise and has only limited experience in this unique kind of relationship building. Adding this capacity to a CSA-led partnership would require training, the development of protocols and the strategic selection of partners.
Limited Managerial Experience with a Healthcare Niche
The Agency's traditional stakeholders came from the space sector, and its programs are typically delivered through transactional dealings with contractors and research entities. Partnering with non-space stakeholders, such as health authorities, healthcare practitioners, patient representatives and Indigenous elders, will require flexible processes and an adaptable culture.
As a government agency, the CSA is transparent and accountable in the way it conducts business. Adherence to the principles of public-sector accountability can result in slower program approvals and implementations than in the private sector. While it will remain transparent and fair, the CSA would also need to support the speed and agility needs of its healthcare and industry partners.
A Smaller Player in Space-Exploration Programs
Despite our global reputation, Canada is one of the smaller players in space exploration. Using per-capita expenditures as a measure of the priority that countries place on space, a study ranks Canada ninth, at US$9 per capita. This is well behind the U.S. (US$125), France (US$49), the United Arab Emirates (US$39) and Russia (US$29). Being a smaller player, our international space partners will question Canada's capacity and ambitions to play a leadership role in deep-space healthcare.
Concluding Remarks
This SWOT analysis represents an inventory of environmental conditions and organizational attributes that could influence the development of a deep-space healthcare initiative in Canada. Upcoming opportunities in space exploration could catalyze benefits for underserved communities on Earth. A suite of national strengths in space operations, national healthcare, training and research represents a solid foundation on which to build an initiative. These opportunities and strengths are to be guarded and bolstered.
There are also threats and weaknesses impeding the vision. While threats cannot be controlled, they must be addressed. Weaknesses should be mitigated through actions to negate their impacts and advance the initiative. For instance, the choice of partners can be strategized to bolster resources and offset weaknesses.
Strengths
- Highly recognized as reliable spacefaring partner
- Specialized expertise in several relevant areas
- Leadership in medical education and practitioner training
- Expertise in advanced healthcare delivery
- Research and academic excellence
- National mindset shaped by geography, climate and diversity
Weaknesses
- Limited internal capacity to engage Indigenous communities
- Limited managerial experience with healthcare niche
- Smaller player in space-exploration programs
Opportunities
- Yearning to venture beyond low-Earth orbit
- Addressing access and medical outcomes for remote and underserved populations
- Rapidly changing needs of aging Canadians
- Healthcare gaps exposed by COVID-19 pandemic
- Synergistic alignment with national priorities
Threats
- Competition for meaningful roles in deep-space healthcare
- Challenging domestic market for healthcare innovation
Chapter 4 - Shaping the Program
In this section
"Discover the force of the skies O Men: once recognised it can be put to use."
With a SWOT inventory in hand, the next step is to develop a structured family of thoughtful and actionable recommendations.
The Advisory Council makes eight recommendations to help the Canadian Space Agency establish a deep-space healthcare program that is nationally critical, visible, scalable, affordable and socially beneficial. All eight are aligned with our proposed vision, mission and values (Chapter 2).
Each recommendation also addresses at least one of the unique factors identified by the SWOT analysis (Chapter 3). Most address several factors. For example, the first recommendation exploits the opportunity to explore space with other spacefaring nations, while building on multiple strengths within Canada's healthcare community.
These recommendations are general in description. Each is therefore broken down into specific actions or tactical steps to facilitate eventual fulfillment of the higher-level strategic objectives.
Recommendation 1
Elevate deep-space healthcare to a strategic priority at the Canadian Space Agency.
Actions
- Working with founding partners and key stakeholders, develop a Roadmap for Action that will translate Agency ambitions and Advisory Council recommendations into coordinated, comprehensive, measurable and sustainable actions.
- Secure the necessary budget and human-resource skill-sets to support a Canadian leadership role in international deep-space medical operations and integration, and to establish a remote healthcare initiative with national partners.
- Establish stakeholder relations and engagement as an essential element of the deep-space healthcare partnership, to raise awareness of space opportunities with external stakeholders and to leverage non-traditional sources of expertise, funding and influence.
Canada's past achievements in space exploration are a result of the government's long-term commitment to the country's space sector, strategic investments in key areas of national strength, as well as the ingenuity of dedicated women and men working at the Agency and elsewhere in Canada's space industry. The strategic importance of Canada's participation in the International Space Station (ISS) is reflected in the magnitude of the CSA's budget and human-resource allocation in activities such as the operation and maintenance of the ISS robotics systems, the astronaut program and life-sciences research and technology-development activities.
At present, there is limited internal capacity for the CSA to sustain another niche area of excellence. The Roadmap for Action will therefore need to include steps leading to ministerial and government approval and funding. An economic and job-creation analysis would set a credible and justifiable path to social benefit, program sustainability and national prosperity. Key stakeholders can assist the CSA to define respective roles and responsibilities for the Agency and its deep-space partners in a national program.
Some current Agency activities will undoubtedly need to be expanded and refocused to better align with this new program priority. For instance, the CSA will need to deepen the resources, expand the partnerships and broaden the mandate and skill-sets of its health and life sciences and operational space medicine groups.
Recommendation 2
Pursue with determination an eventual Canadian leadership role in astronaut healthcare, well-being and performance for deep-space missions, starting with major contributions to the Lunar Gateway and Artemis programs.
Actions
- Engage with NASA senior leadership on Canada's aspiration to provide fundamental health infrastructure and capabilities as a means to enhance crew well-being and performance, reducing mission risk from health-related factors.
- Ensure that upcoming discussions with the government for approval of a deep-space healthcare program include a mandate to negotiate with NASA for an eventual healthcare leadership role.
Sending astronaut crews to Mars and safely returning them will measure the best of humanity's energies and skills. This new class of exploratory missions will be unlike anything NASA or its partners have flown before. Some challenges will be operational; others will be technical. However, the most critical challenge to be addressed before we launch the first mission will be maintaining the health, well-being and performance of these intrepid astronauts. This will have a direct impact on mission success.
In the very near future, NASA is expected to begin seeking commercial and international partners to develop a health maintenance system architecture for Gateway and Artemis. Canada can aspire to play a major role in the long-term development and deployment of these systems. An early role as a strong participant in both of these programs could represent first steps on our longer-term journey to space healthcare leadership.
It will be essential for the CSA to negotiate a Gateway/Artemis role that is substantial and meaningful. Such a position must strategically enhance Canadian capacity and experience in medical operations. Sole contribution of a standalone technology is not endorsed by the Advisory Council; that would do little to advance Canada's longer-term ambitions and provide no social benefit.
Rather, we endorse a system-level contribution of sufficient magnitude and program criticality to warrant a barter for multiple flights for CSA astronauts. The Advisory Council has heard from specialists who highlighted several Canadian strengths in healthcare innovation. Fashioning a contribution upon these competencies would be strategic for longer-term ambitions and transformative for patient care on Earth. We recommend (in order of preference) a complement of the following as contributions to Lunar Gateway/Artemis.
- AI-based health informatics network and data infrastructure
- Provision of a CSA Flight Surgeon as co-chief medical officer in the Gateway/Artemis programs and as inflight medical support
- Designation of the Northern Demonstration Site(s) as the prime program facility for evaluation, integration and qualification of all equipment and protocols, as well as expert-generalist and contextual (lived) experience crew training
- Oversight of crew and mission support training, including provision of simulation and tele-mentoring assets
Additional standalone contributions could include:
- Suite of clinical diagnostics
- Environmental health monitoring sub-system
- Wearable technologies
Recommendation 3
Leverage the vision for human space exploration and deep-space healthcare solutions by transforming healthcare delivery for medically underserved populations.
Actions
- Engage and collaborate with federal, provincial and territorial governments, health authorities and other organizations responsible for healthcare delivery in order to identify and strategically invest in areas at the intersection of deep-space and remote healthcare challenges. Leverage existing pressures into opportunities for positive change by increasing medical autonomy, patient empowerment and equity in access.
- Collaborate with senior First Nations, Inuit and Métis representatives to identify priority healthcare challenges. Consider how deep-space healthcare innovation could address these challenges while ensuring cultural safety.
- Work with organizations that support seniors and caregivers, including industry, community, government, researchers and end-users, to identify priority healthcare delivery challenges. Co-develop shared solutions, with a focus on patient empowerment.
- Embed a focus on frontline practitioners into programmatic considerations and decisions.
Healthcare solutions developed for deep space offer novel opportunities for governments and communities to address the needs of underserved populations. In particular, the CSA should explore opportunities to collaborate with Indigenous peoples and with the many interconnected organizations responsible for their healthcare delivery. These will include federal, provincial and territorial governments, national and local Indigenous organizations, and healthcare authorities.
Many First Nations, Inuit and Métis healthcare inequities are rooted in Canada's colonial past and remaining barriers to reconciliation. In order to respect the Indigenous principle of "nothing about us, without us,
" this initiative must establish relationships with Indigenous partners from the outset. Authentic connections will foster better understanding of Indigenous healthcare and wellness challenges, as well as culturally safe and effective means to address them.
The gap in access to local care, particularly specialized care, is widening for remote communities compared to urban centres.
The physicians and nurses who serve in rural and remote regions of Canada are remarkable professionals – the decathletes of clinical medicine. Broad knowledge and highly honed skills enable them to diagnose and manage a wide range of clinical cases. When faced with uncertainty and ambiguity, the MacGyver-instincts of these expert-generalists allow them to devise novel solutions.
While highly regarded and indispensable to remote healthcare delivery, there are too few practitioners to staff all of our nation's northern medical clinics. Full complements of diagnostic aids and therapeutic equipment are not always available nor straightforward to maintain. Audio, video and data networks that are needed to consult with specialist team members in the south are not dependable. Transportation infrastructure is at the mercy of adverse weather conditions. Understandably, the work of practitioners in remote communities can be challenging, stressful and lonely.
Approaches, technologies and infrastructure must be enhanced to better support these essential members of our healthcare system. Innovations in AI-enabled diagnostics and therapeutics offer hope of improved patient outcomes. Advancements in contextual training, simulation and tele-mentoring for local practitioners could bolster mental and professional resilience. Improvements in communication and transportation infrastructure would enable continuous and reliable connections with supporting consultants at tertiary care centres. Collectively, these measures - not unlike those required for future deep-space healthcare providers - could improve the recruitment and retention of practitioners to communities that sorely need their services.
Another underserved community is Canada's fast-growing cohort of aging baby-boomers. Seniors value their independence and prefer to remain in their homes and communities as long as possible. New models of patient care will be developed in pursuit of this goal. Monitoring and patient-centric solutions derived from deep-space applications could help seniors maintain their autonomy, health and quality of life.
The concept of medical operations for deep space will be based on crew autonomy and patient-centred healthcare (meaning independence from Earth) through advances in technology, training and clinical approaches. The CSA and its collaborators should regard the empowerment of patients and practitioners as a quintessential feature of the initiative. A frontline focus, whether in space or in a remote terrestrial setting, will drive program decisions and success.
Recommendation 4
Build on Canada's unique model of competency- and team-based medical education and its industrial leadership in simulator-based training. Pursue a deep-space leadership role in the development of advanced training and simulation approaches to build, maintain, credential and certify the skills of crew medical officers.
Actions
- Brief senior NASA officials on Canada's leadership and capacity in medical and health sciences curriculum development and simulator-based training. Pursue a role for Canada in the competency- and team-based medical training, certification and credentialling of international crews.
- Engage with Canadian expert-generalist training groups (e.g., curriculum developers, preceptors, researchers, companies) and explore collaborative opportunities on common priorities.
- Leverage Canadian industrial expertise in AI-powered and simulator-based training solutions. Develop AI/VR/AR-enabled tools to train astronauts and remote healthcare practitioners, as well as tools for skills maintenance, just-in-time training and skills refreshment.
Deep-space missions will require at least one onboard crew member with a broad general medical mindset and skills supporting specialist needs. Similarly, remote communities and residences for seniors would better maintain their healthcare autonomy with local care administered by expert-generalists trained with specialist capabilities and technology.
A deep-space healthcare training role for Canada would align well with our national capacity to train rural generalists to work within low-resource regions. Practitioners are trained to a high level in multiple skill-sets, utilizing traditional, virtual and simulator-based methods, while supported by networks of specialists. The CSA should engage with these physician and nurse training institutions, while exploring the feasibility of expanding existing accredited training programs to include a deep-space medical specialty, including team-based support of crew health through networks of specialists.
Recommendation 5
Establish a Northern Demonstration Site Program as a means to test and evaluate remote clinical approaches and innovations, and to nurture fruitful relations with Indigenous communities and other critical stakeholders.
Actions
- Accelerate the establishment of a network of demonstration sites in remote, underserved regions of Northern Canada. Working with local practitioners, these sites would validate and demonstrate the utility of Canadian and international healthcare innovations that could enable deep-space healthcare and be transformative for the delivery of remote terrestrial care. Utilize the sites to train deep-space astronauts as well as remote-care specialists in clinical skills as well as essential traits, such as resourcefulness.
- Prior to the design and development of the Northern Demonstration Site program, perform a needs analysis. Include considerations of Indigenous community partnerships in this analysis, as well as the engagement of local practitioner and other remote health stakeholders, the incorporation of AI-enabled innovations, and team-based approaches to healthcare delivery through networks of specialist coaches, tele-mentoring and broadband connectivity.
- Develop terms of participation jointly with Indigenous leaders and elders and local nursing/medical staff where the Northern Demonstration Sites will be located. Principles of participation for the community should respect:
- Local history and current means of healthcare delivery
- Co-development of the mandate, scope, research agenda, operations and impact of the demonstration sites
- A community share in the ownership of the local site
- Governance over the health and research data as well as visitors to the community
- In partnership with local leadership, offer access to the Northern Demonstration Sites to international partners for assessment and advancement of their deep-space approaches, training and technologies. Consider how space solutions could address community healthcare and wellness challenges. Offer access to national researchers and entrepreneurs as a means to develop and refine commercial prototypes.
In collaboration with northern communities and elders, the CSA should quickly establish a Northern Demonstration Program, with a series of sites in suitable northern remote settings. Among other functions, these sites would serve as medical testbeds to pilot essential approaches, protocols, practitioner training and technologies that enable deep-space missions. These would include:
- Autonomous and semi-autonomous systems (diagnostic and therapeutic)
- Patient-centric technologies
- Point-of-care technologies
- Virtual-care approaches (e.g., tele-mentoring and just-in-time training)
The CSA's existing relationship with the University of British Columbia, University of Northern British Columbia, health authorities, Indigenous health leaders and rural healthcare stakeholders in Northern British Columbia should support its consideration as the initial Northern Demonstration Site. Once this site is running well, the program could expand to other northern locations and Indigenous communities.
The full participation of the local population and engagement of regional and Indigenous health authorities will facilitate two-way exchanges of ideas and enhance each site's effectiveness and sustainability.
Recommendation 6
Leverage the combined expertise and capacity of Canada's research and innovation communities and the health and biomedical technology sector to accelerate the development of solutions for deep-space healthcare challenges.
Actions
- Explore collaborative opportunities with universities, as well as public and private research and innovation organizations, to:
- Incentivize and enhance mechanisms for meaningful engagement with academic leaders and teams
- Establish the capacity to identify and nurture a broad network of exploration and clinical researchers and innovators
- Discuss with prospective innovation partners (see Appendix G) ways to engage a broader spectrum of Canada's researchers, innovators and entrepreneurs in the CSA's research opportunities, to incentivize the community in its R&D funding opportunities, and streamline application processes
- Formalize collaborative agreements between the Deep-Space Healthcare Program and prospective granting councils (see Appendix G), and discuss access to aligned funding programs and other granting mechanisms.
- Explore partnerships with organizations in the health and biomedical sector that accelerate innovation and foster collaboration between industry and researchers, to translate emerging research and technology into applied healthcare delivery problems, including the management of chronic-care patients and seniors.
- Review lessons learned from healthcare delivery gaps exposed by the COVID-19 pandemic. Review spaceflight approaches and technologies that could enhance emergency preparedness and improve healthcare responses to marginalized populations in future health crises.
Healthcare innovation today is achieved through multi-sectoral, multi-disciplinary collaboration. Canada has a strong reputation in health and medical research and a well-established federal research and innovation ecosystem, which works together to enable the creation of research partnerships and the sharing of knowledge between academic institutions and the private sector. Furthermore, the Canadian medical technologies industry is supported by incubators, accelerators and other research networks.
These entities work collaboratively to advance innovation and help companies grow and scale through the provision of valuable advice, direction, resources and funding. They facilitate the integration of leading-edge solutions in the delivery of healthcare. Collectively, this innovation community could form a strong national partnership in deep-space and remote healthcare.
Recommendation 7
Exploit Canada's expertise and capacity in artificial intelligence to develop remote healthcare solutions in space and on Earth.
Actions
- With artificial intelligence (AI) partners, initiate prototyping of an advanced AI-enabled health informatics network to support the preventive, predictive, diagnostic and therapeutic functions of a remote healthcare facility. Include clinical diagnostic, decision-support and wearable technologies in the system.
- As a means to build credibility and gain valuable experience as a leader, technology integrator and trainer, explore and invest in the development of a medical data architecture to be used in Northern Demonstration Sites and scaled up for future space missions.
- Collaborate with leaders of the AI-for-Health community in Canada to pursue aligned opportunities. For instance, a medical data architecture could be evaluated in the Northern Demonstration Program for potential application in underserved communities where local healthcare expertise and patient-centric care are valued.
AI does not yet have the capability to diagnosis medical syndromes, but it can augment the diagnostic capabilities of a crew medical officer. AI and other digital technologies will support the autonomy requirements of deep-space operations. New diagnostic tools and treatments enabled by AI will improve the effectiveness, efficiency and safety of onboard health management. AI-in-health technologies will inform disease prevention and support the development of remote-healthcare solutions.
Although solutions to the global warming-related health crisis will be complex, computer-based technologies will likely form the basis of solutions. Healthcare technologies developed for a deep-space healthcare program will be valuable in supporting such Earth-based health needs. Capabilities of remote physiologic monitoring through wearable devices and networked communications, for example, will provide innovative approaches to solving some of these health challenges.
Recommendation 8
Develop a Canadian public outreach strategy and cultural exchange focused on remote healthcare in space and on Earth.
Tactical Steps
- Develop a strategic outreach and education program that targets all Canadians, especially youth and seniors. This will demonstrate the importance of CSA activities in the development of new and innovative approaches to deliver healthcare from coast to coast to coast, noting the potential to create viable, versatile career opportunities and lasting social change.
- In partnership with Indigenous communities, co-develop culturally relevant programs that incorporate Indigenous approaches to education and that engage Indigenous youth in the adventure of deep-space exploration.
- Solicit fresh perspectives and new ideas using innovative funding tools, such as national challenges, to generate innovative solutions that benefit both people on Earth and astronauts in space.
The ability of the CSA to showcase the achievements of our astronauts and various space technologies is renowned. Past initiatives with the public have brought our nation together and built pride. The next decade in space will present even more opportunities for the Agency to elevate its public outreach objectives to higher levels.
We encourage the Agency to exploit new collaborations with non-traditional healthcare partners by extending the reach of its existing outreach programs and engaging even more youth. In particular, the daunting nature of deep-space missions will appeal to the innate fascination of youth with exploration. It will be an unprecedented opportunity to engage with First Nations, Inuit and Métis students from coast to coast to coast to encourage the acquisition of STEM skills and the pursuit of career dreams in healthcare delivery and innovation. Working in collaboration with the CSA, Indigenous education organizations and other likeminded partners could use the opportunity to take their education initiatives into the far corners of Canada.
The Apollo moon landings sparked curiosity and inspired the global public to redefine what it considered possible. Participation in the next phase of exploration will brand Canada internationally as a nation of explorers and innovators. And in an age of reconciliation, it will be an unprecedented opportunity for Canadians to come together and engage in cultural exchanges and two-way conversations over the societal roles of exploration, innovation and education.
Chapter 5 - Building the Team
In this section
"If you want to go fast, go alone. If you want to go far, go together."
The Roles and Responsibilities of a Partnership
A deep-space astronaut healthcare initiative would be a significant undertaking for the CSA, as the Agency does not have sufficient expertise and resources to take this on alone. The pursuit of such an audacious goal would require an extraordinary and unprecedented collaboration among government agencies, healthcare agencies, academic institutions, the commercial sector, technology companies, communities and Canada's health innovation ecosystem.
Membership would be rationalized around the partnership's expected roles and responsibilities. On behalf of NASA and other international space partners, this Canadian partnership would aspire to leadership in flight operations, crew training and sub-systems integration. This would be a substantive role—on par with Canada's traditional oversight of robotic systems and operations for the space shuttle, International Space Station and Lunar Gateway programs.
This partnership would co-develop novel approaches for spaceflight to improve the delivery of healthcare on Earth and catalyze their adoption in underserved communities. For instance, advanced training methods and facilities commonly used to prepare astronauts for flight could be incorporated into the instruction of remote healthcare practitioners. Similarly, the partnership could co-develop monitoring technologies and patient-centric approaches that would be applicable to the clinical management of both deep-space astronauts and chronic-care patients.
To undertake these functions, we recommend an interdisciplinary, well-resourced, multi-sectoral, highly networked partnership. Membership composition would be a key enabler of program success.
To provide the necessary breadth of expertise and resources, this partnership should include pertinent sectors of the space, technology and healthcare ecosystems:
Government Departments
Federal, provincial and territorial jurisdictions that oversee healthcare policy, regulations and budgets.
Health-Delivery Agencies
Provincial and territorial health authorities are the operational element of Canada's healthcare system. They deliver coordinated care across a broad range of services, from prevention and primary care to quaternary and long-term care. They oversee an impressive array of facilities, tools, systems, policies, funding and personnel.
Frontline Healthcare Practitioners
Frontline healthcare practitioners are the nurses, physicians, midwives, community-health workers and pharmacists who deliver essential health services directly to patients in their communities. They are trusted sources of information in remote and other underserved settings, and have skills in preventing, treating and managing a variety of illnesses. Aboard a deep-space vehicle, the frontline worker is the physician-astronaut designated as the crew medical officer.
In this partner sector, we also include the academic institutions (medical schools, nursing schools, hospitals) and professional associations responsible for the training and support of frontline practitioners.
Research Institutions
Research-intensive universities and research institutes, hubs and accelerators conduct research and provide training in health and biomedical disciplines. Granting councils support R&D and facilities related to health, well-being and associated technologies.
Industry
Companies develop and produce goods and services in the space, health, technology and medical fields. Industry associations enable collaboration and foster overall development of the sector.
Indigenous and Other User Communities
The user community includes residents of rural and remote communities who are disadvantaged by limited access to tertiary-care facilities and medical specialists, new Canadians who are isolated by language and culture, chronic-care patients and long-term care residents. In particular, the key user community is Indigenous peoples who experience numerous barriers to healthcare in rural/remote as well as urban settings. Aboard a deep-space vehicle, the user community is the astronaut crew.
International Partners
International partners include space agencies such as NASA and ESA that would collaborate with the CSA and Canadian participants in the delivery of deep-space healthcare.
Each sector possesses unique strengths and could contribute leveraged funding or in-kind services. Collectively, this partnership would become a formidable national collaboration.
Ideal Partner Attributes
The Advisory Council considered attributes that characterize an ideal partner and bring together the depth, breadth and credibility of a national collaboration. Those qualities would ensure the partner:
- Would fulfill a role vital to the mission of the partnership
- Has the ability to remain committed over the long term
- Would contribute expertise and other resources
- Has an organizational mandate aligned with the mission of the partnership
- Would be willing to share the risks of the initiative and to develop opportunities
- Has influence with national decision-makers
Value Propositions
The envisaged deep-space healthcare partnership must be beneficial to all parties.
Partners will naturally ask, "What's in it for us?
" The answer will vary from partner to partner. Below are value propositions for different categories of stakeholders, foreseen as incentives to committing resources to this deep-space healthcare initiative.
Government Departments
- Shared solutions to shared challenges – Deep-space healthcare technologies, developed and validated on Earth, have tremendous potential to benefit Canadians from underserved communities, in particular remote Indigenous communities. An autonomous, decentralized approach to healthcare can help improve health access, equity and outcomes for underserved populations.
- Economic and social benefits At both the national and community levels there will be benefits from the creation of desirable healthcare technology, gains in employment and improvements in community resilience, autonomy and stability.
Health-Delivery Agencies
- Cost control – Healthcare delivery costs are constantly increasing. In particular, many territorial governments must provide patients with transportation to distant tertiary clinical centres for specialized services, at great expense. The need for medical transportation would be reduced by enabling monitoring, diagnosing and treatment of patients in their communities or at home.
- Human resources – Recruitment and retention of healthcare practitioners and staff is difficult, especially in remote settings, even with financial incentives. Meaningful collaboration in a deep-space initiative, combined with upgraded training and care networks, would encourage a steady, sustained source of human resources for remote settings and hard-to-reach urban populations.
Frontline Healthcare Practitioners
- Telemedicine support – Remote healthcare providers would benefit from improved telemedicine protocols linking them with colleagues in tertiary centres, given improved access to broadband and other networking technologies.
- Simulation, training and clinical decision support – Access to high-quality simulation and virtual training, as well as AI-enabled clinical decision-support tools, would broaden the spectrum of care available to remote communities by local practitioners.
Research Institutions
- Reputational Gain – Research institutions would see their global credibility and reputation enhanced by collaborations with CSA, NASA and other international agencies, as well as engagements with non-traditional partners.
- Funding Opportunities – Dedicated research funds would open opportunities for new research programs across Canada, furthering the national culture of innovation.
- Talent Recruitment – Exciting research and academic opportunities would attract top international graduate students and postdoctoral fellows. There would be enhanced training opportunities, internships and employment for students.
Industry
- Innovation – Canadian companies would develop cutting-edge technologies addressing unmet needs in both the healthcare and space markets and gain competitive edge.
- Access to Resources – Small- and medium-sized companies would have an opportunity to gain access to accelerator testbeds for evaluation of their prototypes, and benefit from financial incentives.
Indigenous and Other User Communities
- Empowerment – Local communities and practitioners would enjoy enhanced decision-making autonomy as well as access to collected data and authority over its use. Self-determination is important to Indigenous peoples; being able to co-develop solutions and partner to bring enhanced health outcomes through improved access and empowering local health professionals is paramount. Enhancing autonomous care would reduce the need for health-related travel, which is expensive and disruptive to patients' lives.
- Social Benefit – There is an opportunity to bring practical and sustainable benefit to communities in terms of healthcare and connectivity, as well to train, employ and mentor the next generation of Indigenous professionals and leaders.
International Partners
- A Trusted Team Player – The CSA has gained a solid reputation as a trusted, reliable partner within the international space community. In activities ranging from research to operations, Canada delivers, and does so in a transparent and collaborative way. Existing partnership agreements with Canada set a precedent for future agreements.
- Technological Expertise – Canada is known for excellence in clinical research, technologies and innovation. In particular, it has significant expertise in AI, with access to a large pool of talent in this field.
Partnership Roadmap
The partnership roadmap described in the following paragraphs consists of proposed activities for the short, medium and long term.
The membership of core partners proposed by the Council at first is deliberately small. The pressing short-term needs of the initiative would demand particularly agile partners renowned for "forming, storming, norming and performing.
"
A list of additional members for consideration, as well as a brief description of their envisioned roles, is provided in Appendix G. We do not specify a medium- or long-term timeframe for their inclusion. As the innovation ecosystem will continue to evolve over the following years, with different and emerging healthcare players, the membership composition of the longer-term partnership can remain flexible at this time.
Nevertheless, the organizations we list for later inclusion are key stakeholders with similar visions, missions and values. They have a reputation for developing novel initiatives on the edge of healthcare innovation. While not formalized at the outset as partners, they should be regarded as allies. It would benefit the deep-space healthcare partnership in its early years to continually reach out to these stakeholders to explore synergies and nurture relationships. They represent a significant depth and breadth of expertise, resources and credibility.
The Short Term: A Core of Founding Partners
In its first two years, the partnership would work toward realization of the near-term goal: For the federal government to designate deep-space healthcare as Canada's next exploration priority. Securing this level of support from government decision-makers is critical.
Associated with the pursuit of this primary goal are a series of enabling tasks.
Priority Near-Term Tasks:
- Formalize deep-space healthcare as a strategic priority at the CSA
- Develop a Roadmap for Action to advance national capability, capacity and credibility in remote healthcare delivery
- Prepare an economic and job-creation analysis for a deep-space healthcare initiative
- Secure a substantial and meaningful healthcare role for Canada on Lunar Gateway/Artemis
- Establish a remote medical infrastructure and Northern Demonstration Site #1 to pilot novel clinical approaches (autonomy, point-of-care, patient-centric, virtual care), training and integration of new technologies and innovations
- Bolster the deep-space healthcare ecosystem
- Develop stakeholder relations and public outreach
With these considerations in mind, the Advisory Council recommends that a deep-space healthcare partnership be initiated around a small group of founding partners. Of particular note, it should involve early, full and active inclusion of Indigenous participants as founding partners.
A listing of these candidate organizations and brief descriptions of their envisioned roles are provided in Appendix G. The pressing nature of the initiative's near-term goal requires that initial partners be agile, dynamic and able to hit the ground running.
The Medium Term: Scaling up Activities and the Partnership
Once the federal government has committed its support for the program, the partnership would focus on its next activities. In the medium term (approximately -) the primary goal would be for NASA to designate Canada to a leadership role in deep-space healthcare.
A slate of tasks aligned with this new goal would focus on enhancing Canada's medical operations experience.
Priority Medium-Term Tasks:
- Contribute Canadian technology, staff and training system to the Lunar Gateway/Artemis programs
- Establish Northern Demonstration Sites #2 & #3
- Establish the deep-space healthcare partnership (management, administration, scale-up)
- Effect knowledge translation to underserved communities
- Broaden the research mandate of the CSA's health and life sciences group
To accomplish this expanded slate of functions, the partnership would require an additional infusion of expertise, effort and commitment. This enlarged partnership would leverage broader medical and innovation resources in pursuit of this medium-term goal.
The Long Term: Further Scaling of the Partnership
Once the goal of securing a leadership role in deep-space healthcare has been realized, the partnership would again expand. Now fully resourced, the partnership would oversee and implement Canada's substantive role and responsibilities in deep space.
The long-term goal of the partnership is to support the health, well-being and performance of crews going to Mars and other destinations in deep space, and to ensure the translation and adoption of knowledge and technologies developed for these space missions in user settings on Earth.
Priority Long-Term Tasks:
- Develop a deep-space healthcare program management team at the CSA
- Establish a world-class program for training & certification of
- Crew
- Support personnel
- Contribute to deep-space healthcare system integration & oversight with international partners
- Establish a continuous presence of mission operations
- Provide resources for Canadian-based technology design, development & testing
- Foster R & D opportunities across Canada
Chapter 6 - Mobilizing the Nation
In this section
"We shall not cease from exploration / And the end of all our exploring / Will be to arrive where we started / And know the place for the first time"
Critical, Visible, Scalable, Affordable and Socially Beneficial
In the terms of reference for the Advisory Council, the Canadian Space Agency asks us to define a program that is "nationally critical, visible, scalable, affordable and socially beneficial.
" What a tall order! While at first glance this requirement appears unrealistic and onerous, the deep-space healthcare program we outline indeed checks all of these boxes.
Critical
Future space missions will encounter risks, harsh environments and operational challenges not previously found in low-Earth orbit. The most daunting challenge for the global space community will be the need to deliver healthcare to onboard crews. In fact, maintenance of the health, well-being and performance of astronauts will be directly tied to mission success. Leadership in deep-space healthcare would be a critical role for Canada.
Visible
Landing astronaut crews on Mars and returning them safely back to Earth will be one of the greatest achievements of the 21st Century. A meaningful role for Canada in this venture would instill national pride and build public excitement. Our expertise in healthcare—clinical research, digital health, medical robotics—would be showcased internationally. Simulators for the training of crew and ground-support personnel, as well as national facilities for system integration and mission operations, would provide high profile.
Scalable
The Advisory Council has proposed a phased approach to the establishment and expansion of the deep-space healthcare partnership, as program milestones are attained. Starting with a core membership, it would grow in ensuing years in its goals, functions, staffing and operating budget.
Program infrastructure (testbeds, training simulators, flight-control consoles) would also be scaled up over time. Demonstration sites would eventually be established in select First Nations, Inuit and Métis communities to catalyze the adoption of novel healthcare delivery models in underserved regions.
Affordable
A Canadian deep-space healthcare initiative cannot cure all that ails the country's healthcare system. The social determinants of health (factors such as housing, income, education, employment, social support networks) have the greatest bearing on health outcomes of marginalized populations and are beyond the scope of a CSA-led healthcare initiative. Nevertheless, approaches associated with the delivery of healthcare to deep-space astronauts could lead to lower medical costs and better health outcomes on Earth. Healthcare costs in Canada exceed $265 billion annually and are rising alarmingly. Patients in remote northern communities must often travel to tertiary-care centres in the south, at a total cost of several hundreds of millions of dollars per year. Empowering local practitioners and clinics with virtual-care support, autonomous and point-of-care technologies has the potential to reduce transportation costs, while building up community-based care.
Socially Beneficial
Improvements in the delivery of healthcare in rural and remote regions and among other medically isolated populations are a national social and economic need. Senior citizens make up 17% of the Canadian population and comprise the fastest-growing segment of our society, yet our healthcare system is not designed to address their changing needs. Seven million Canadians—19% of our population—live in rural or remote regions. They are served by just 8% of Canadian physicians. While urban Canadians enjoy world-class medical care, these people do not. Morbidity and mortality rates among northern Canadians are well above the standards of OECD countries.
Shortcomings in access, equity and healthcare outcomes are particularly acute for Indigenous peoples. The report of the Truth and Reconciliation Commission of Canada identifies health inequities as a specific and critical call to action, to "identify and close the gaps in health outcomes between Aboriginal and non-Aboriginal communities… [including] the availability of appropriate health services.
" A role in deep-space healthcare could become an adjunct to focus attention on the delivery of remote healthcare. Training methodologies developed to support crew medical officers on deep-space missions could be translated to empower physicians and nurses working in remote regions. Appendix H provides several clinical vignettes that illustrate how terrestrial applications could arise from medical technologies developed for deep space.
Similar to the era of the Apollo Moon landings, the public could be emboldened by the audacity of deep-space exploration to address other seemingly insurmountable societal challenges—climate change, food security, global mental health. The next generation of youth could be inspired to pursue STEM educational paths and seize career opportunities in healthcare and innovation.
Keys to Success
The Advisory Council has outlined an initiative at the crossroads of space exploration and remote healthcare. Our report is admittedly lengthy and the many programmatic considerations we present are likely overwhelming. As we conclude, it may be helpful to highlight a handful of factors—the most salient points—that the Advisory Council considers to be keys to program success.
Systems Mindset
Healthcare, in any setting, is head-spinning in its complexity. Multiple healthcare jurisdictions exist within Canada, each with its own legislative, policy, regulatory and licensing requirements. Other considerations include patient access, equity and outcomes; privacy, quality control and safety standards; and supply chains and global markets.
At the centre of all this are frontline practitioners. Their ability to manage the health, well-being and performance of their patients is enabled by curriculum, training, simulators, procedures, communication networks, facilities and tools. In addition to physicians, these practitioners also include nurses, biomedical engineers, scientists, physiotherapists, chronic-care coordinators, mental-health specialists, dieticians and pharmacists.
An undertaking in remote healthcare—whether in deep space or in underserved communities—will necessitate a systems-level management style. An initiative led by the Canadian Space Agency would not be simply a research and development program. Technology development, in fact, would be the easy part. The hard part of remote healthcare will be coordinating the spectrum of innovations, partners, jurisdictions, training, procedures and support personnel to form an integrated system around the crew medical officer in deep-space or the frontline practitioner in an isolated part of Canada.
Mobilizing the Nation
Government space agencies have traditionally contracted with domestic industry or research institutions to deliver equipment or services to global exploration programs. To enable Canada's contribution to deep-space healthcare, the Advisory Council has proposed a different approach. We suggest that an alliance of partners—not contractors—develop opportunities, share risks and deliver solutions.
This notion of an alliance resonates with candidate partners. Prior to publication of this report, the Advisory Council met individually with several candidate partner organizations. As we briefed them on the CSA vision for deep-space healthcare and the work of our Council, we sensed a buzz of excitement. All organizations were intrigued by the audacity of the vision and the nature of the partnership. They understood how participation could benefit their own organizational mandate, and agreed that a collaboration spanning space, innovation, training and healthcare sectors would be formidable.
Be aware that there will be competition from international space agencies for the leadership role in deep-space healthcare. Leadership would bring significant benefits to any nation, enhancing its reputation, economy and innovation ecosystem, and become a highly regarded niche of spaceflight competence.
However, the notion of a national partnership would differentiate a Canadian bid for leadership in deep-space healthcare from those of competing space agencies. In essence, the full might of Canada's publicly funded healthcare system—accounting for 12% of our GDP—as well as the country's deep pools of research and industrial expertise would be brought to bear. A cross-disciplinary, well-resourced, highly networked national alliance would represent a competitive edge. A multinational collaboration to explore deep space could also benefit from quintessential Canadian leadership traits: Equity, diversity and inclusion; multiculturalism; openness and fairness; diplomacy; collaboration; reliability; good government and a spirit of exploration.
Integrating the Partners
Invention, it is said, often resides at the intersection of cross-disciplinary expertise. But management of a dynamic, multi-sectoral entity may be challenging. Much like an international astronaut crew, a deep-space healthcare partnership will bring together organizations of disparate expertise, cultures, perspectives, practices and governance. During the early years, managers will therefore need to devote time and effort to communicate clearly, build relationships, adapt processes and work smoothly across the founding membership.
Large transformational initiatives of the past have often relied on the services of system integrators to bring together diverse players and contributions. These management firms facilitate collaboration among players by maximizing synergies and ensuring that overarching systems (e.g., digital information networks) function seamlessly. If the CSA is not resourced to oversee partner integration, then the services of an established integrator firm could be sought as a means to de-risk the initiative.
A Sense of Urgency
A final key to success will be to quickly build capability, credibility and experience in deep-space medical operations.
The Advisory Council does not endorse continued middling contributions by Canada to international space programs, with self-congratulatory statements that we punch above our weight. Canada has been a respected, but minor, participant in past human spaceflight partnerships. We must do better. The current low flight-rate of CSA astronauts is inadequate to sustain a vibrant spaceflight program, showcase national innovations, capture public interest and inspire the next generation of leaders.
Rather, the Advisory Council endorses significant investment by Canada in deep-space healthcare in order to enlarge its sphere of international influence, to better position our nation among spacefaring peers, to assume a role critical to human spaceflight and to play a key part in unlocking the mysteries of the solar system.
Having been one of the smaller players in space exploration, we can expect that international space partners will question Canada's capacity to assume a lead role. There will therefore be an urgent need for Canada to secure a strategic system-level contribution to the Lunar Gateway/Artemis programs and then, in the following years, to build on national capability, credibility and experience in medical operations.
The Last Word
Leading such a transformative program would bolster Canada's reputation as a nation of explorers. Yes, there will be many issues to address, including budgetary concerns, programmatic risks, heightened scrutiny and partner relations. But a deep-space healthcare program could become a rallying grand challenge for our nation.
Wayne Gretzky has said that we miss 100% of the shots we don't take. The Advisory Council regards deep-space healthcare as a loose puck before a gaping net. We are enthusiastic about the potential of this initiative to empower exploration by astronauts of the inner solar system and to improve patient outcomes on Earth. Canada could become the global leader in remote healthcare.
References
In this section
- References DEDICATION
- References CHAPTER 1 – GRASPING THE TORCH
- References CHAPTER 2 – LAUNCHING THE VISION
- References CHAPTER 3 – SCANNING THE ENVIRONMENT
- References CHAPTER 4 – SHAPING THE PROGRAM
- References CHAPTER 5 – BUILDING THE TEAM
- References CHAPTER 6 – MOBILIZING THE NATION
- References APPENDIX B – CLINICAL, BIOMEDICAL AND PERFORMANCE NEEDS OF DEEP-SPACE MISSIONS
The Advisory Council benefitted from consulting a wide range of publications, articles and online resources. Many of these are listed according to the chapters and sections of the report where they proved useful.
DEDICATION
- Dr. A. Maxwell House brought health care to remote places. The Globe and Mail. Obituary published , Joan Sullivan.
CHAPTER 1 – GRASPING THE TORCH
- The Global Exploration Roadmap. NP-2018-01-2502-HQ. Washington, DC: National Aeronautics and Space Administration Headquarters, .
- Global Exploration Roadmap – Supplement – Lunar Surface Exploration Scenario Update. NP-2020-07-2888-HQ. Washington, DC: National Aeronautics and Space Administration Headquarters, .
- Pathways to Exploration – Rationales and Approaches for a U.S. Program of Human Space Exploration. ISBN 978-0-309-30507-5. Washington, DC: National Academies Press, .
- Exploration, Imagination, Innovation: A New Space Strategy for Canada. Cat. No. ST99-60/2019E-PDF. Her Majesty the Queen in Right of Canada, .
- Canadian Healthcare in Deep Space: Advancing our country's leadership in autonomous care in space and on Earth. Report of the Expert Group on the Potential Canadian Healthcare and Biomedical Roles for Deep-Space Human Spaceflight. Cat. No. ST99-61/2019F-PDF. Her Majesty the Queen in Right of Canada, .
CHAPTER 2 – LAUNCHING THE VISION
- Building Your Company's Vision. Harvard Business Review. Boston, MA. Jim Collins and Jerry I. Porras, .
- Leading Change: Why Transformation Efforts Fail. Harvard Business Review. Boston, MA. John P. Kotter, .
CHAPTER 3 – SCANNING THE ENVIRONMENT
Opportunities
- The Global Exploration Roadmap. NP-2018-01-2502-HQ. Washington, DC: National Aeronautics and Space Administration Headquarters, .
- Global Exploration Roadmap – Supplement – Lunar Surface Exploration Scenario Update. NP-2020-07-2888-HQ. Washington, DC: National Aeronautics and Space Administration Headquarters, .
- Prospects for Space Exploration: An economic and strategic assessment of the space exploration sector. 2nd edition. Paris, France. Euroconsult, . Available online at: https://digital-platform.euroconsult-ec.com/wp-content/uploads/2020/07/SPX20_Brochure.pdf
- Euroconsult Releases its Government Space Programs Report – Expenditures Reach US$70.9 Billion in . SpaceQ. Marc Boucher, . Available online at https://spaceq.ca/euroconsult-releases-its-government-space-programs-report-expenditures-reach-us70-9-in-2018/
- Review of Family Medicine Within Rural and Remote Canada: Education, Practice, and Policy. College of Family Physicians of Canada; Mississauga, ON. Carmela Bosco and Ivy Oandasan, .
- Rural Opportunity, National Prosperity: An Economic Development Strategy for Rural Canada. Cat. No. T94-13/2019E-PDF. Her Majesty the Queen in Right of Canada, .
- Delivering more equitable primary health care in Northern Canada. Canadian Medical Association Journal 189(45): E1377-8. T. Kue Young and Susan Chatwood, .
- Addressing provider turnover to improve health outcomes in Nunavut. Canadian Medical Association Journal;191(13): E361-4. Maria Cherba et al., .
- Canada's elder care crisis: Addressing the doubling demand. A report by Deloitte and commissioned by the Canadian Medical Association, .
- How Home-Based Primary Care Can Reduce Expensive Hospitalizations. Harvard Business Review. Boston, MA. Paul Di Capua et al., .
- As COVID-19 exposes long-term care crisis, efforts grow to keep more seniors at home. CBC News. Toronto. Nicole Ireland and Natalie Kalata, .
- Optimizing Access to Heart Failure Care in Canada During the COVID-19 Pandemic. Canadian Journal of Cardiology, 36(7), 1148-1151. Sean Virani, et al., .
- Canada's Unequal Health System May Make Remote Indigenous Communities More Vulnerable To The Coronavirus. The Conversation. Ann Seymour, .
- How To Build A Better Canada After COVID-19: Make Telehealth The Primary Way We Deliver Health Care. The Conversation. Ahmad Firas Khalid, .
- Coronavirus: New Technologies Can Help Maintain Mental Health In Times Of Crisis. The Conversation. Stéphane Vial, .
- National Survey of Canadian Physicians – use of digital health and information technology among physicians in Canada – Report. Canada Health Infoway and Canadian Medical Association. Leger, .
- Canada's Superclusters: Right people. Right place. Right time. Government Canada, . Available online at https://www.ic.gc.ca/eic/site/093.nsf/eng/home
- Innovation For A Better Canada. Government Canada, . Available online at https://www.ic.gc.ca/eic/site/062.nsf/eng/home
- Federal Government Commits Additional $250 Million In IRAP Funding To Support High Growth Startups. Canadian Startup News. Meagan Simpson, .
- Minister Of Indigenous Services Mandate Letter. Office of the Prime Minister, . Available online at https://pm.gc.ca/en/mandate-letters/2019/12/13/minister-indigenous-services-mandate-letter
- How should we act on the social determinants of health? Canadian Medical Association Journal 190 (42): E1241-2. Trevor Dummer, .
- United Nations Declaration on the Rights of Indigenous Peoples. UN General Assembly, . Available online at https://www.un.org/development/desa/indigenouspeoples/declaration-on-the-rights-of-indigenous-peoples.html
- Unleashing Innovation: Excellent Healthcare for Canada. Report Of the Advisory Panel on Healthcare Innovation. Cat. No. H22-4/9-2015E-PDF Her Majesty the Queen in Right of Canada, .
- Canada's universal health-care system: achieving its potential. The Lancet. 391(10131): 1718-1735. London, UK. Danielle Martin et al., .
- Pan-Canadian Artificial Intelligence Strategy. CIFAR, . Available online at https://www.cifar.ca/ai/pan-canadian-artificial-intelligence-strategy
- Ecological dynamics across the arctic associated with recent climate change. Science. 325(5946): 1355-8. Eric Post et al., .
- Dangerous climate change and the importance of adaptation for the Arctic's Inuit population. Environ Res Lett. 4(2). James Ford, .
Threats
- Development Of an Accepted Medical Condition List for Exploration Medical Capability Scoping. NASA/TM-2019-220299. Houston, TX. Rebecca Blue, Derek Nusbaum and Erik Antonsen, .
- Recommendation for a Medical System Concept of Operations for Gateway Missions. Document developed by the Exploration Medical Capability Element's Systems Engineering team. HRP-48012. Houston, TX. David Rubin, .
- Unleashing Innovation: Excellent Healthcare for Canada. Report Of the Advisory Panel on Healthcare Innovation. Cat. No. H22-4/9-2015E-PDF Her Majesty the Queen in Right of Canada, .
- Enabling health technology innovation in Canada: Barriers and facilitators in policy and regulatory processes. Health Policy, 123(2), pp.203-214. Maggie MacNeil et al., .
- Health and Biosciences: The sector today and opportunities for tomorrow. Interim Report of the Health/Bio-sciences Table of Canada's Economic Strategy Tables. Karimah Es Sabar et al., .
- Digital Industries: The sector today and opportunities for tomorrow. Interim Report of the Digital Industries Table of Canada's Economic Strategy Tables. Tobias Lütke et al., .
- Canada has long way to go on virtual care. Canadian Medical Association Journal 192(30): E227-8. Lauren Vogel, .
- The Innovation Dilemma: Achieving Value, Health Outcomes and Contributing to the New Economy. The Future of Medical Technology in Canada. Publication produced by OPTIMUS | SBR on behalf of MEDEC, the national association representing Canada's medical technology industry, .
- The Health Costs of Climate Change: How Canada Can Adapt, Prepare, and Save Lives. Canadian Institute for Climate Choices. Ottawa, ON. Dylan Clark et al., .
- Changes in Canada's Regions in a National and Global Context. Chapter 8 in Canada's Changing Climate Report, pp. 424-443. Cat. No. En4-368/2019E-PDF. Her Majesty the Queen in Right of Canada, represented by the Minister of Environment and Climate Change, . Stewart Cohen et al., .
Strengths
- International Cooperation. NASA. Mark Garcia and Brian Dunbar, . Available online at: https://www.nasa.gov/mission_pages/station/cooperation/index.html
- Canada Joins NASA's Lunar Gateway Station Project With 'Canadarm3' Robotic Arm. Space.com. Elizabeth Howell, .
- Invest in Canada: Canada's Robotics Industry. Cat. No. FR5-38/25-2016E-PDF. Her Majesty the Queen in Right of Canada, .
- The Global Partnership on Artificial Intelligence officially launched. Montréal International, . Available online at: https://www.montrealinternational.com/en/news/the-global-partnership-on-artificial-intelligence-officially-launched/
- Canadian Healthcare in Deep Space: Advancing Our Country's Leadership in Autonomous Care in Space And on Earth. Report of the Expert Group on the Potential Canadian Healthcare and Biomedical Roles for Deep-Space Human Spaceflight. Cat. No. ST99-61/2019F-PDF. Her Majesty the Queen in Right of Canada, .
- A proposal for the curriculum and evaluation for training rural family physicians in enhanced surgical skills. Canadian Journal of Surgery, 58(6), pp.419-422. Nadine Caron, Stuart Iglesias, et al., .
- Joint position paper on rural surgery and operative delivery. Canadian Journal of Rural Medicine, 20(4), pp. 129-138. Stuart Iglesias et al., .
- Fifty Years On: A Retrospective on the World's First Problem-based Learning Programme at McMaster University Medical School. Health Professions Education, 5(1), pp. 3-12. Virginie Servant-Miklos, .
- The Future Of Medical Education In Canada: A Collective Vision for MD Education. The Association of Faculties of Medicine of Canada, .
- The Future Of Medical Education In Canada : One vision forward - Reigniting our common vision for the Future of Medical Education in Canada. The Association of Faculties of Medicine of Canada, .
- There's An AI Revolution Underway and It's Happening in Canada. Forbes. Jersey City, NJ. Bijan Khosravi, .
- Toronto's thriving AI ecosystem serves as a model for the world. VentureBeat. San Francisco, CA. Naheed Kurji, .
- World's First All-Robotic Surgery Performed in Canada. ZDNet. Andrew Nusca, .
- Competing in a Global Innovation Economy: The Current State of R&D in Canada. Report of the Expert Panel on the State of Science and Technology and Industrial Research and Development in Canada. Cat. No. T177.C2C68 . Council of Canadian Academies, Ottawa, .
- QS World University Rankings by Subject : Life Sciences & Medicine. Available online at https://www.topuniversities.com/university-rankings/university-subject-rankings/2021/life-sciences-medicine
- QS World University Rankings by Subject : Nursing. Available online at https://www.topuniversities.com/university-rankings/university-subject-rankings/2021/nursing
- A Canadian Take on the International Patient Engagement Revolution. Healthcare Quarterly 21 (Special Issue). Toronto, ON. Vincent Dumez and Antoine Boivin, .
Weaknesses
- Indigenous health research and reconciliation. Canadian Medical Association Journal 191 (34): E930-1. Marcia Anderson, .
- Indigenous health disparities: a challenge and an opportunity. Canadian Journal of Surgery 61(5): 300-301. Alika Lafontaine, .
- The mirage of universality: Canada's failure to act on social policy and health care. Canadian Medical Association Journal 192 (5): E105-6. Andrew Boozary and Andreas Laupacis, .
CHAPTER 4 – SHAPING THE PROGRAM
Recommendation 1
- Canadian Healthcare in Deep Space: Advancing our country's leadership in autonomous care in space and on Earth. Report of the Expert Group on the Potential Canadian Healthcare and Biomedical Roles for Deep-Space Human Spaceflight. Cat. No. ST99-61/2019F-PDF. Her Majesty the Queen in Right of Canada, .
Recommendation 2
- How NASA Uses Telemedicine to Care for Astronauts in Space. Harvard Business Review. Boston, MA. Anil Menon et al., .
- Defining the specialist generalist: The imperative for adaptive expertise in family medicine. Canadian Family Physician. Mississauga, ON. Nicole Woods et al., .
Recommendation 3
- Challenge Ahead: Integrating Robotics, Artificial Intelligence and 3D Printing Technologies into Canada's Healthcare Systems. Standing Senate Committee on Social Affairs, Science and Technology. Her Majesty the Queen in Right of Canada, .
- Socio-Economic Benefits Study of Deep Space Health Care Solutions Used in Northern and Remote Communities. Euroconsult and Leap Biosystems, .
Recommendation 4
- Simulation in education for health care professionals. BC Medical Journal 57 (10): 444-448. Elspeth McDougall, .
- A proposal for the curriculum and evaluation for training rural family physicians in enhanced surgical skills. Canadian Journal of Surgery, 58(6): 419-22. Nadine Caron et al., .
- Doctors need retraining to keep up with technological change. Canadian Medical Association Journal 190(30): E920. Lauren Vogel, .
- Training the Next Generation of Doctors and Nurses. New York Times Nov. 4, page L4. Laura Pappano, .
- Research: How Virtual Reality Can Help Train Surgeons. Harvard Business Review. Boston, MA. Gideon Blumstein, .
Recommendation 5
- Space medicine innovation and telehealth concept implementation for medical care during exploration-class missions. Acta Astronautica. Amsterdam. Annie Martin et al., .
- 3D printers: A revolutionary frontier for medicine. The Conversation. Toronto, ON. Ivar Mendez, .
- Canadian national survey of point-of-care ultrasound training in family medicine residency programs. Can Fam Physician 64(Oct): e462-7. Taft Micks et al., .
Recommendation 6
- Investing in Canada's Future: Strengthening the Foundations of Canadian Research. Report of the Advisory Panel for the Review of Federal Support for Fundamental Science, . ISBN 9780995924.
- Building A Learning Health System for Canadians. Report of the AI for Health Task Force. CIFAR, . Available online at https://www.cifar.ca/ai/pan-canadian-artificial-intelligence-strategy/building-a-learning-health-system-for-canadians
Recommendation 7
- 10 Promising AI Applications in Health Care. Harvard Business Review. Boston, MA. Brian Kalis et al., .
- An emotionally intelligent AI could support astronauts on a trip to Mars. MIT Technology Review. Neel V. Patel, .
- Canada has a chance to monopolize the artificial intelligence industry. The Globe and Mail, Toronto, ON. John Kelleher and Laura McGee, .
- How Artificial Intelligence Could Help Hospitals Save Lives. The Walrus. Toronto, ON. Conor Lavelle, .
Recommendation 8
- Equity, Diversity, and Inclusivity in Science, Technology, Engineering, and Mathematics: Forging Paths to Enhanced Innovation. Roundtable Summary Report. Ryerson University, Toronto, ON. Imogen R. Coe and Mehrdad Hariri, .
CHAPTER 5 – BUILDING THE TEAM
- Managing Partner Relations in Joint Ventures. MIT Sloan Management Review. Cambridge, MA. Bettina Büchel, .
- 3 Ways to Build a Culture of Collaborative Innovation. Harvard Business Review. Boston, MA. Kate Isaacs and Deborah Ancona, .
- Developmental sequence in small groups. Psychological Bulletin, 63(6), 384-399. B. W. Tuckman, .
- The Rural Road Map for Action – Directions. Mississauga, ON: Advancing Rural Family Medicine: The Canadian Collaborative Taskforce; .
- Care close to home: Progress on the Rural Road Map. Canadian Family Physician 65(Oct): 760. Francine Lemire, .
- Progress made on access to rural health care in Canada. Canadian Family Physician 66(Jan): 31-36. Ruth Wilson et al., .
- COVID-19 and the decolonization of Indigenous public health. Canadian Medical Association Journal 192(38): E1098-1100. Lisa Richardson and Allison Crawford, .
- Indigenous-led health care partnerships in Canada. Canadian Medical Association Journal 192(9): E208-16. Lindsay Allen et al., .
- Virtual Care in Canada: Discussion Paper. Canadian Medical Association Health Summit. .
- Engagement of nurse practitioners in primary health care in northern British Columbia: a mixed-methods study. Canadian Medical Association Journal Open 9(1): E288-94. Erin Wilson et al., .
CHAPTER 6 – MOBILIZING THE NATION
- Truth and Reconciliation Commission of Canada (TRC). Honouring the truth, reconciling for the future. Summary of the final report of the Truth and Reconciliation Commission of Canada. Montréal: McGill-Queen's University Press, .
APPENDIX B – CLINICAL, BIOMEDICAL AND PERFORMANCE NEEDS OF DEEP-SPACE MISSIONS
- Principles of Clinical Medicine for Space Flight. Springer, New York, NY. Michael Barratt (ed.) et al., .
Glossary
We have attempted to write this report in a style that is appealing and understandable to a lay audience. However, there are occasional references to spaceflight, innovation and healthcare terminology that may not be familiar to all readers. For clarity, definitions of several terms are provided. Furthermore, many terms have varied meanings in the open literature, depending on context. The terms listed below are defined as we associate them with a deep-space healthcare initiative.
- Accelerator
-
An innovation accelerator is a growth program that provides support to a validated business concept in order to scale quickly. This support can be in the form of resources (people and money), mentors, connections and knowledge. An accelerator can help start-ups grow to a stage where they acquire customers and are ready to take on additional investment and/or be acquired.
- Artificial Intelligence (AI)
-
Artificial intelligence or AI refers to the capability of a machine to imitate some aspects of human intelligence. In its broadest meaning, AI is defined as the theory and development of computer systems able to perform tasks that normally require human intelligence. Examples of such tasks include visual perception, speech and text recognition, correlations, decision-making and language translation. For example, in healthcare, an artificial virtual assistant (like Siri or Alexa) can have conversations with practitioners and patients about lab results and clinical next steps.
- Artemis Program
-
Artemis is the new U.S. lunar human exploration spaceflight program. It is led by NASA, with participation from the U.S. spaceflight industry and several international partners who are signatories to the Artemis Accords and who establish formal bilateral agreements with NASA. Artemis aims to return humans to the Moon for the first time since the Apollo program, specifically to the lunar south pole region. A stated goal is to land the first woman astronaut and visible minority astronaut there in this decade. Long-term goals include establishing a sustainable human presence on the Moon, laying the foundation for private companies to build a lunar economy and eventually sending humans to Mars.
- Autonomy
-
Medical autonomy in space describes the need for humans to operate independently from terrestrially based medical support. The treatment of all conditions when communication latency to Earth is greater than 20 minutes should be considered autonomous. Closely allied to space medical autonomy is access to local healthcare for underserved populations on Earth. Autonomy can also have an ethical connotation, denoting a patient's right to be involved in the management of their own healthcare.
- Deep Learning
-
Deep learning is an area of machine learning that attempts to mimic the activity in layers of neurons in the brain to learn how to recognize complex patterns in data. The "
deep
" in deep learning refers to the large number of layers in neurons in contemporary machine-learning models that help to learn rich representations of data to achieve better performance gains. - Deep Space
-
Deep space is the region of space beyond low-Earth orbit and, in particular, that part of the inner solar system beyond the Earth-Moon system.
- Digital Health
-
Digital health is the integration of digitized health data, automated processes, decision-support tools and analytics with the use of audio, video and other technologies to deliver preventive, predictive, diagnostic and treatment services that promote patient and population health. Software applications and services are typical digital deliverables.
- Expert-Generalist
-
An expert-generalist is a physician or nurse whose clinical practice is not limited to a narrow focus. Rather, their training, skills and contextual judgment enable them to diagnose and manage a variety of clinical problems - from routine and simple problems to unusual and highly complex cases. The broad expertise (emergency medicine, anaesthesia, enhanced surgical skills), resourcefulness and inventiveness of expert-generalists make them well-suited for practice in rural and remote settings on Earth and in deep-space.
- Expert Group
-
The Expert Group on the Potential Canadian Healthcare and Biomedical Roles for Deep-Space Human Spaceflight is a previous task force of the Canadian Space Agency. It published its findings in a report. The overall counsel of the Expert Group was that the CSA and a group of aligned national partners should secure a role in the coming years as an international leader in deep-space astronaut healthcare. Lessons learned from developing new approaches, training and technologies for deep space could be translated to improve the delivery of healthcare to underserved regions of our nation. More background information is provided in Appendix E.
- Frontline Health Workers
-
Frontline workers deliver essential health services directly to patients in their communities, especially, for the purposes of this report, in rural and remote areas. They include nurses, physicians, midwives, community-health workers and pharmacists. They are trusted sources of information and have skills in preventing, treating and managing a variety of illnesses. They are able to identify conditions that require higher levels of care and facilitate referral.
Aboard a deep-space vehicle or habitat, the frontline workers will include the physician-astronaut designated as the crew medical officer (CMO), as well as non-physician astronauts qualified as paramedics.
- Global Exploration Roadmap
-
The Global Exploration Roadmap (GER) is a publication () of the International Space Exploration Coordination Group (ISECG), a forum of space agencies. It describes a non-binding, long-range strategic plan to explore the inner Solar System in a sustainable fashion. It shares a vision for human and robotic space exploration, beginning with the International Space Station and extending to the Moon, asteroids, Mars and other destinations. The GER emphasised international collaboration based upon a common set of exploration goals, objectives and identified benefits to humanity.
Building on the edition and on growing global interest in space exploration, a recent supplement () updates the Roadmap with the latest developments in lunar exploration planning in an updated lunar surface exploration scenario.
- Health Authority
-
Provincial and territorial governments are responsible for the delivery of healthcare to their residents. Health authorities (or health regions) are the management model used by these jurisdictions to administer and deliver public health. Most health authorities are organized along geographic boundaries, however some work along operational lines. Some provinces such as Alberta and Saskatchewan have one health authority, while others such as Quebec have several. British Columbia has a dedicated First Nations Health Authority.
- Health Beyond and Health Beyond Team
-
Health Beyond is Canada's deep-space healthcare initiative. The Health Beyond team supported the work of the Advisory Council on Deep-Space Healthcare. Members were matrixed together from several divisions of the Canadian Space Agency and Indigenous Services Canada. In addition to advancing the deep-space healthcare initiative, the team provided administrative, communication, workshop facilitation, analysis and writing support to the Advisory Council.
- Incubator
-
An innovation incubator is a growth and mentoring program that gives early-stage start-ups access to investors, logistical support such as shared office space, technical resources and other assistance to help get established. Some incubators operate as non-profit organizations, while others provide seed capital and support in exchange for some ownership in the business. Companies that use an incubator have innovative ideas that are still defining their goals, business models and product/market fit. (Companies that have moved beyond the incubator stage use business accelerators for support.)
- Indigenous Peoples
-
Indigenous (Aboriginal) peoples are the original inhabitants of Canada. The Constitution recognizes three distinct Indigenous groups—First Nations, Métis and Inuit. First Nations and Inuit history extends well before the arrival of Europeans in Canada, while Métis emerged as a distinct culture after intermarriage between European settlers and First Nations people. There are 1.7 million Indigenous peoples in Canada. Although they represent just 4.9% of the population, they occupy a significant proportion of Canada's land mass and coastal areas, as determined by modern-day land claims and historical treaties.
Indigenous peoples live throughout Canada and strive to reinvigorate traditional culture and ways of life. Some Indigenous communities are located within urban centres, but many are on their designated lands. First Nations, Inuit and Métis communities situated in rural and remote locations bear a disproportionate burden of poor health outcomes, best understood through the lens of the social determinants of health, especially colonization. The current government, the CSA and its partners are committed to work with Indigenous peoples to provide culturally safe, people-specific, self-determined care.
While some Indigenous peoples share a number of common attributes, each population has distinct cultures and sub-cultures. A distinctions-based approach is essential when collaborating with communities and elders.
- International Space Exploration Coordination Group
-
The International Space Exploration Coordination Group (ISECG) is a voluntary, non-binding forum of 26 space agencies working to advance the Global Exploration Strategy through coordination of mutual efforts in space exploration. A key product of the Group is the Global Exploration Roadmap.
- Low-Earth Orbit
-
Low-Earth orbit (LEO) is a region of near-Earth space extending from an altitude of 160 km above Earth's surface to 1,000 km above Earth's surface. It is the space where most artificial satellites for communications, remote-sensing and navigation orbit. The International Space Station also flies in LEO, in an orbit of about 400 km. With the exception of the Apollo lunar missions from - , all human spaceflights to date have been in LEO.
- Lunar Gateway
-
The Lunar Gateway will be a small, modular space station orbiting the Moon, to be constructed in the next few years. It will be assembled by NASA in collaboration with international (CSA, ESA, JAXA) and commercial partners. The Gateway will support short-term orbital missions and astronaut excursions by serving as a communications hub, science laboratory, habitation outpost and storage facility.
- Machine Learning
-
Machine learning is a subset of AI that often uses statistical techniques to give machines the ability to "
learn
" from data without being explicitly given the instruction for how to do so. This process is known as "training
" a "model
" using a learning algorithm that progressively improves model performance on a specific task. Reinforcement learning is an area of machine learning concerned with developing software agents that learn goal-oriented behaviour by trial and error in an environment that provides rewards or penalties in response to the agent's actions (called a "policy
") toward achieving that goal. - Northern Communities
-
Northern communities lie within the northern territories of Canada, which include Yukon, Northwest Territories and Nunavut. This region accounts for 39% of Canada's landmass but just 0.32% of the country's population. Not all northern communities are considered remote, for example the city of Whitehorse has a population of 22,000. Northern communities are typically very different both from each other and from their southern counterparts, but they also possess some common attributes.
- Partner
-
A deep-space healthcare partner has an organizational mandate closely aligned with the mission of the partnership. It fulfills a role vital to the success of the program. It contributes significant direct funding, expertise or resources.
- Patient-Centric Care
-
In patient-centric care, the patient is a key member of the healthcare team. This will be particularly true in the remote setting of a deep-space outpost where crewmembers will play a collaborative, coordinated role with the rest of the medical support cadre on Earth. Due to communication latencies and the non-real time nature of virtual consultations, deep-space astronauts will be trained and resourced to take more responsibility for the management of their own health and well-being. Personal medical information will be accessible and onboard medical facilities will be designed so that astronauts can monitor their physiology and make informed decisions.
- Point-of-Care Testing
-
Point-of-care testing refers to medical diagnostic investigations performed outside a clinical laboratory or tertiary-care centre, most often at the patient's bedside.
- Primary Care
-
Primary care is the day-to-day healthcare given by a physician (general practitioner or family physician), physician assistant, nurse, nurse practitioner or community health worker. Typically, this provider acts as the first contact and principal point of continuing care for patients within a healthcare system. The role of primary care is to promote health, prevent disease and identify diagnostic, curative, rehabilitative, supportive and palliative services required by the patient. These services may be provided in a physician's office, nurse-practitioner's office, community-health centre or nursing station.
- Quaternary Care
-
Quaternary care is an advanced level of care that is highly specialized and not widely accessible. Examples of quaternary services are experimental medicine, the treatment of rare conditions and some types of uncommon diagnostic or surgical procedures. These are usually offered only in a limited number of regional or national healthcare centres.
- Rural and remote communities
-
The Statistics Canada definition of a rural or small town is the population living in a town or municipality outside the commuting zone of larger urban centres that have populations of 10,000 or more people.
A remote community is defined as a community located more than 350 km from the nearest service centre with year-round road access. In many cases, remote communities are not accessible by road or rail, only by air or sea. While remote communities are not homogeneous, they share access and staffing challenges and are dependent on the weather.
Indigenous Services Canada uses four levels of remoteness to classify the access of First Nations communities to health services:
- Type 1: Remote isolated – No road access, no scheduled flights, minimal telephone and radio access
- Type 2: Isolated – No road access, scheduled flights, good telephone services
- Type 3: Semi-isolated – Road access to physician services at a distance greater than 90 kilometres
- Type 4: Non-isolated – Road access to physician services at a distance less than 90 kilometres.
- Rural and Remote Medicine
-
Rural and remote medicine is practiced outside of urban areas, where most care is provided by a small number of physicians or nurse practitioners with limited or distant access to specialist resources and high-technology healthcare facilities. The remote location of the practice obliges the practitioners to have scopes of practice and procedural skills not usually required in urban practice.
Remote practitioners can provide primary, secondary and at times tertiary care. They work collaboratively with a local team of healthcare providers. Consultations with specialists by phone, in person, by videoconference or through transfer of patients to urban centres enables quality care to be offered to people who live in remote communities.
- Social Determinants of Health
-
Social determinants of health are non-medical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live and age, and the wider set of forces and systems shaping the conditions of daily life. The list includes but is not exclusive to:
- Housing, basic amenities and the environment
- Food Insecurity
- Education
- Income and social protection
- Social Inclusion and non-discrimination
- Access to affordable health services of decent quality
Social determinants of health can have a major impact on people's health and well-being and contribute to health disparities and inequities among marginalized populations. For example, people who don't have access to grocery stores with healthy foods are less likely to practice good nutrition. That raises their risk of health conditions like heart disease, diabetes and obesity, and even lowers life expectancy relative to people who do have access to such foods.
- Stakeholder
-
A stakeholder organization plays a role that is important but not considered vital to the sustainability of the deep-space healthcare initiative. While the organization may contribute in-kind expertise and resources, a stakeholder does not assume program risk and is not formally committed to the partnership.
- SWOT
-
A SWOT framework is a strategic analysis tool used to assess an organization's or department's internal capabilities (Strengths, Weaknesses) as well as the external environment in which it operates (Opportunities, Threats).
- Systems Management
-
A systems management approach considers all the relevant elements that must interact in order to effectively address healthcare delivery challenges. It integrates information, technologies, services, policies and other elements with the participating organisations that, in turn, may be part of other systems.
A systems approach does not deliver solely technical solutions; rather, it ensures the orderly alignment of software, hardware and processes in an innovative manner to address pressing health challenges. Most importantly, an effective healthcare system approach is centred on people, their needs and capabilities.
- Tertiary Care
-
Tertiary care is specialized healthcare for inpatients in an academic teaching hospital or large community-care facility. Such care is typically provided by specialists with access to specialized equipment for advanced medical investigation and treatment. Examples of tertiary-care services are cancer management, neurosurgery, cardiac surgery, burn treatment and specialized neonatology services, as well as other complex medical and surgical interventions.
- Underserved Communities
-
Underserved communities are geographic regions, usually rural and remote, that experience difficulty recruiting and retaining adequate health personnel to meet the needs of the population, or that are undersupplied with certain health services.
Underserved populations experience difficulties in access to medical care given the geographic region where they live, because of lower educational or socioeconomic status or other barriers. They may also receive less care, a lower standard of care or treatment that does not adequately meet their needs. They are at risk of sub-standard health outcomes. Underserved populations include Indigenous peoples, refugees, immigrants who do not speak either of Canada's official languages, the elderly, people with disabilities and those with alternate lifestyles.
- Valley of Death
-
In the health innovation world, "
valley of death
" is the metaphor used to describe the gap between a research discovery and its commercial application in the marketplace. It is where many promising innovations wither and die before they can be proven or advance far enough to attract investment funds. This valley exists in part as a result of difficulties in implementing, accelerating or financing an innovation project. Grants from funders of biomedical research generally focus on basic research. However, new tools, platforms and products often require expensive animal and/or clinical trials before investors commit. The discoveries therefore remain unfunded, unfinished and stranded. - Venture Capital and Capitalist
-
Venture capital (VC) is a form of private equity financing to start-ups and early-stage companies that have demonstrated high growth or have high growth potential. The start-ups are usually based on an innovative technology or business model. The invested capital is known as venture capital and the investing individuals or firms are called venture capitalists. In essence, the venture capitalist takes on the risk and invests in an entrepreneur's idea, in exchange for equity or an ownership stake. This nurtures the start-up for a short period of time until it reaches a sufficient size and credibility and then exits, with the help of an investment banker.
- Virtual Care
-
Virtual care (or telehealth) refers to interactions between patients located remotely and their healthcare providers, using digital and communications technologies. Examples of virtual care include medical consultations, mobile-health monitoring of home-based chronic-care patients and even telesurgery. The aim of virtual care is to maximize the quality and effectiveness of patient care. It can help deal with the increase in demand for home- and facility-based continuing care as the Canadian population ages.
Acronyms and Abbreviations
This report includes the acronyms and abbreviations defined below:
- 3-D
-
Three-dimensional
- AI
-
Artificial Intelligence
- Amii
-
Alberta Machine Intelligence Institute
- AR
-
Augmented Reality
- CEO
-
Chief Executive Officer
- CFI
-
Canada Foundation for Innovation
- CIFAR
-
Canadian Institute for Advanced Research
- CIHR
-
Canadian Institutes of Health Research
- CMA
-
Canadian Medical Association
- CMO
-
Crew Medical Officer
- CPAC
-
Canadian Partnership Against Cancer
- CRCC
-
Canada Research Coordinating Committee
- CSA
-
Canadian Space Agency
- ESA
-
European Space Agency
- FNHA
-
First Nations Health Authority
- F/P/T
-
Federal, Provincial and/or Territorial jurisdictions
- G7
-
Group of Seven – an intergovernmental organization consisting of Canada, France, Germany, Italy, Japan, the UK and the U.S.
- G20
-
Group of Twenty – an international forum for the governments and central bank governors from 19 countries and the European Union
- GDP
-
Gross Domestic Product
- GER
-
Global Exploration Roadmap
- iHAB
-
International Habitation Module of the Lunar Gateway station
- IT
-
Information Technology
- ISC
-
Indigenous Services Canada
- ISED
-
Ministry of Innovation, Science and Economic Development
- ISECG
-
International Space Exploration Coordination Group
- ISS
-
International Space Station
- LEAP
-
Lunar Exploration Accelerator Program
- LEO
-
Low-Earth Orbit
- Mila
-
Montreal Institute for Learning Algorithms
- NASA
-
National Aeronautics and Space Administration
- NRC
-
National Research Council of Canada
- NSERC
-
Natural Sciences and Engineering Research Council of Canada
- OECD
-
Organisation for Economic Co-operation and Development
- QS
-
Quacquarelli Symonds world university rankings
- R&D
-
Research and development
- SME
-
Small- and medium-sized enterprise
- SRPC
-
Society of Rural Physicians of Canada
- SSHRC
-
Social Sciences and Humanities Research Council of Canada
- STEM
-
Science, Technology, Engineering and Math
- SWOT
-
Strengths, Weaknesses, Opportunities and Threats
- UN
-
United Nations
- UNESCO
-
United Nations Educational, Scientific and Cultural Organization
- VC
-
Venture Capital
- VR
-
Virtual Reality
Appendix A Human Exploration Plans for Deep Space
In this section
A.1 International Space Exploration Coordination Group
In , the international space exploration community came together with a shared vision for what will follow the International Space Station (ISS), with the aim of expanding human presence beyond low-Earth orbit. The International Space Exploration Coordination Group (ISECG) was formed. Canada was a founding partner and today serves as its chair.
The ISECG keeps expanding its membership, attesting to the growing interest in space exploration. At the time of writing, there are 26 member agencies.
A.2 Global Exploration Roadmap
ISECG regularly updates and issues a consensus Global Exploration Roadmap (GER). The third edition of the GER was released in . Its main elements are:
- Continuing the development of ever-more reliable life-support and other space technologies using the ISS and various Earth-based analogues.
- Building the Lunar Gateway, a mini-space station in lunar orbit, accessible with the spacecrafts of the Artemis program.
- Returning humans to the surface the Moon, initially as sorties from the Gateway and eventually with a more permanent outpost on the Moon's surface.
- Enabling a pathway to human missions to Mars, drawing on the technologies developed for the above missions.
A supplement to the GER was released in Summer , with the latest updates reflecting the current focus on preparing for lunar surface operations and integrating emerging commercial capabilities among ISECG participating countries.
A.3 Lunar Gateway and Canadarm3
The Lunar Gateway is a NASA-led international collaboration. The proximity of the Moon, just three days away, makes it a relatively safe setting to test novel technologies and space systems for future deep-space missions, in particular with respect to human health and habitation impacts.
Planned as a mini space station on a highly elliptical lunar orbit, Gateway will provide a base for sustainable, long-term exploration of the Moon. When fully assembled, it will support a crew of four astronauts, who will live and work at the outpost for up to three months at a time. The Gateway will also serve as a staging platform for robotic and human sorties to the lunar surface. Unlike the ISS, Gateway will not host crews on a permanent basis. For that reason, it will be highly automated.
Assembly will happen in stages. The completed outpost will include a power and propulsion module, a habitation and logistics module, a communications module, docking ports, an airlock for spacewalks and Canadarm3, Canada's contribution. This highly autonomous robotic system will use advanced machine vision and advances in artificial intelligence (AI) to perform tasks without human intervention, ensuring safe and sustainable operations of Gateway.
A.4 Artemis Program
The goal of the Artemis program is to return humans to the Moon in a sustainable way within this decade, in preparation for the human exploration of Mars. Its main components are a powerful new rocket, the Space Launch System; a deep-space capsule, the Orion Spacecraft; and a Moon Lander.
The Artemis I mission, scheduled for , is to be an uncrewed test flight to lunar orbit. The first crewed test flight, Artemis II, scheduled two years later, is to send astronauts on an eight-day journey around the Moon and back to Earth, testing the capabilities of the Orion Spacecraft and collecting valuable flight test data. The four-person crew of Artemis II is to include a CSA astronaut, making Canada only the second country after the U.S. to send an astronaut into deep space.
The subsequent Artemis III mission is to land the first woman astronaut and first visible minority astronaut on the Moon. That four-person crew is to initially dock with the Lunar Gateway. Two of the astronauts are to then fly a lander to the Moon's south pole, where they are expected to spend a week exploring the Moon's surface and performing scientific experiments.
Follow-on missions will be either to the Gateway, as a terminus, or they will use it as a base for sorties to the lunar surface. Canada has secured a further flight for a CSA astronaut to the Lunar Gateway, at a date still to be determined.
The next planned phase will be the gradual development of surface infrastructure, leading eventually to an autonomous Moon base with a focus on mobility, exploration and science, with an eye to creating a viable lunar economy.
Note: the Artemis program is not to be confused with the Artemis Accords, an international agreement signed in by Canada, the U.S., Australia, Italy, Japan, Luxembourg, the United Arab Emirates and the UK that establishes how countries can cooperate to peacefully and responsibly conduct exploration of the Moon.

Lunar surface exploration plan phases. (Credit: NASA)
Lunar surface exploration plan phases - Text version
NASA's Artemis program will return humans to the Moon and prepare us for the next giant leap - the exploration of Mars. Artemis is focused on accomplishing an initial human landing by mid-decade, while simultaneously working toward a sustainable exploration capability by the late 2020s.
The powerful Space Launch System (SLS) and Orion spacecraft, Starship Human Landing System, Falcon Heavy and other commercial launch vehicles will provide the rocket power needed to transport humans back to the Moon and to construct lunar outposts. Infrastructure will be built up incrementally over the next decade:
- Commercial Lunar Payload Services
-
The Commercial Lunar Payload Services program will provide commercial delivery of small and medium payloads to the lunar service. Initial investigations will study the lunar surface and resources at the lunar poles.
- Artemis I
-
The uncrewed, maiden flight of the integrated SLS rocket and Orion spacecraft in will target a distant retrograde orbit around the Moon. The 3-week flight will evaluate spacecraft performance and test Orion's heat shield during its high-speed reentry back to Earth at 2,700 degrees Celsius.
- Artemis II
-
The first crewed flight of SLS/Orion will send four astronauts, including a CSA crewmember, on a lunar flyby mission in . During this 10-day test flight, astronauts will validate deep space communication and navigation systems and assess the ability of life support systems to keep them healthy and safe.
- Gateway
-
The Gateway orbiting outpost will establish a human presence in the vicinity of the Moon for NASA and international partners. The Power and Propulsion Element and the Habitation and Logistics Outpost will be the first modules of the Gateway to be launched. On later missions, crew residing on the completed station will conduct research and from there venture down to the surface.
- Initial Human Landing System
-
The commercially-provided Human Landing System will transport crew down to the lunar surface and, at the end of their surface explorations, return them back to lunar orbit. The initial landing system will provide access to the surface for two crew, with later, more sustainable landers accommodating four crew on the surface.
- Artemis III
-
Orion and a crew of four will launch from Earth in and rendezvous with the Human Landing System in lunar orbit. A female and male astronaut will then board the Lander and descend to the surface. The two crewmembers will explore the lunar surface in new exploration spacesuits (xEMUs) for about a week before rejoining their crewmates in lunar orbit for the trip back home aboard Orion.
- Surface Mobility
-
The Lunar Terrain Vehicle (i.e., unpressurized rover) is the surface transportation system for the lunar landing mission. Use of this vehicle will extend the range of explorations by the crew, and thereby enable more scientific research and resource prospecting. In later years, NASA and its partners will develop an Artemis Base Camp at the lunar South Pole. Base Camp infrastructure will also include a Lunar Terrain Vehicle. During non-crewed periods, the Vehicle will be tele-operated to support surface research and to transport small deployable payloads around nearby sites.
A.5 Journey to Mars
The exploration of Mars has been a goal of space programs for decades. Using the GER as a guide, the international partners are working toward this long-term goal alongside the fast-growing commercial space-exploration sector. An ambitious timeline has been set, with the first humans on the surface of Mars by the end of the 2030s, likely preceded by robotic missions to prepare for their arrival.
The challenges of such a mission are daunting, from its stunning technological and operational complexity to the incredible risks of this hostile space environment. Sustained human presence in the lunar environment will be key to testing, demonstrating and mastering the systems needed for this journey, using the Moon as a Mars analogue to progress toward independence from Earth. Managing the threats of prolonged space exposure to human health and performance and enabling crew medical autonomy is seen as a key challenge to the success of these ambitious and perilous missions. This is where the importance of an envisaged role for Canada in deep-space healthcare lies.
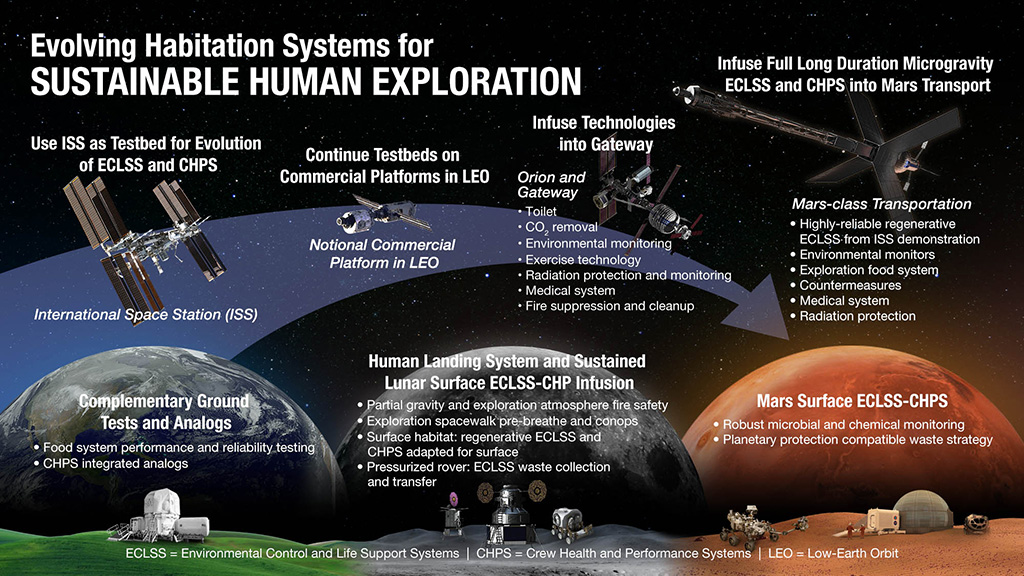
Overview of systems for sustainable human exploration. (Credit: NASA)
Lunar surface exploration plan phases - Text version
Advancements in spacecraft habitation systems will ensure a safe living environment as well as the health and well-being of astronaut crews who will participate in future exploratory missions to deep space. NASA and its partners have already begun to upgrade existing systems using a variety of ground- and space-based testbeds. Lessons learned are being used to incrementally advance technologies needed to enable missions to the next destination. In a sense, new habitation capabilities will be tested and validated in a series of missions like stepping-stones on the way to Mars.
- Use ISS as Testbed for Evolution of ECLSS and CHPS
-
The International Space Station (ISS) remains the primary testbed for validating the Environmental Control and Life Support System (ECLSS), the Crew Health and Performance System (CHPS) and other key habitation technologies. Ongoing testing aboard the ISS will provide the necessary capability and confidence for a sustained human presence far beyond low-Earth orbit.
- Complementary Ground Tests and Analogs
-
Terrestrial analog sites (such as the Human Exploration Research Analog at the NASA Johnson Space Center) and ground-based testing are complementary to the ISS. They are currently being used to determine reliability predictions and identify areas for system improvement.
- Continue Testbeds on Commercial Platform in LEO
-
Commercial space stations in Low-Earth Orbit (LEO) will continue the system validation work that was begun on the ISS. These future platforms will conduct the necessary long-duration testing and thereby aid the understanding of system reliability and the prediction of needed spares.
- Human Landing System and Sustained Lunar Surface ECLSS-CHP Infusion
-
Intermittently-crewed surface missions over a range of lunar latitudes will demonstrate closed life support systems that are adapted for partial gravity. Robust EVA interfaces to address the lunar dust environment and to isolate spacewalking crew from surface contamination will also be assessed.
- Infuse Technologies into Gateway
-
Orion and Gateway missions will encompass initial short sorties and facilitate the testing of a variety of habitation sub-systems such as the toilet, CO2 removal and environmental monitoring. Gateway architecture will initially incorporate open loop ECLSS, but will then evolve to become more representative of future Mars missions. Gateway will provide access to the unique deep space radiation environment - important for assessment of system controller electronics and some Crew Health and Performance Systems.
- Infuse Full Long Duration Microgravity ECLSS and CHPS into Mars Transport
-
Transit missions to Mars will require greater ECLSS closure to markedly reduce consumption of water and oxygen. High reliability of space flight hardware will be essential for these missions where all spares must be launched with the transit vehicle.
- Mars Surface
-
Ultimate advancements in ECLSS and CHPS technologies will be needed to enable long duration missions without options for resupply or medical evacuation. Out of concern for planetary protection, life support systems must be near-closed loop to preclude surface contamination by the generation of habitat waste products.
Appendix B Clinical, Biomedical and Performance Needs of Deep-Space Missions
In this section
B.1 Current Concept of Operational Space Medicine
Since the dawn of space exploration, specialists in space medicine have addressed the implications of spaceflight on the health of astronauts. Their objectives are threefold:
- To optimize the health and fitness of astronauts prior to flight
- To provide healthcare during flight, maintaining crew well-being and performance, both physically and mentally
- To provide post-flight rehabilitation to life back on Earth
This field is known as operational space medicine. Significant strides have been made in care-delivery and research, with clinicians and biomedical engineers successfully developing countermeasures to deal with most medical problems related to spaceflight. This effort is intended to minimize the overall mission risk, by addressing the so-called "human system risk
". Research is targeted to mitigate the effects of spaceflight on human health and helps inform spacecraft designers and mission planners how to best protect crews and optimize their performance.
Until now, medical care in space has been based on the concept of telemedicine, with the overall health of crew members supervised by teams on the ground. Care is managed from the mission control centre by the Flight Surgeon, a physician specialized in the care of space crews, with the support of biomedical engineers and a network of subspecialist consultants.
Expected and routine disorders are diagnosed and treated onboard by an astronaut with advanced medical training, designated as the crew medical officer. Rarer or more complicated issues are managed in coordination with the ground by the Flight Surgeon's team. This is made possible with abundant real-time voice communication between the ground and the crew, facilitated by the high-bandwidth transmission of health data.
Should there be a critical medical situation that cannot be readily resolved in space, the ill crew member would first receive stabilizing treatment onboard and then be returned to Earth for definitive care. This "stabilization and transportation
" concept has fortunately not been required to date, but it is an option, given the relative proximity of the ISS to Earth.
B.2 Crew Health and Performance on Deep-Space Missions
The current model will not work once astronauts venture beyond Earth's orbit for prolonged periods to the Moon's surface, Mars and beyond. These new class of missions will take astronauts beyond a practical point of no return. The Moon is some 1000 times farther from Earth than the ISS and Mars is some 1000 times farther than the Moon.
Deep-space missions will exacerbate physical and psychological stressors already present on the ISS:
- Communications delays, with a one-way latency of up to 20 minutes for voice and data transmission between Earth and Mars
- No option for medical evacuation, given distance
- Longer duration: A round-trip mission to Mars, for example, is envisaged to take two-and-a-half years, while typical ISS expeditions last about six months
- After having adapted to micro-gravity for the duration of the transit, upon landing on a planetary or lunar surface, the crew will need to adjust to the partial gravitational environment and then adapt to microgravity again on the way back home
- Limited mass, volume and power-allowances of onboard equipment and systems
- Exposure to high levels of ionizing radiation beyond Earth's protective magnetic field
- Consumption of long shelf-life, processed food
- Continuous loud ambient noise from onboard equipment
- Limited crew size
- Stress of extreme isolation and confinement
- Risk of mood disorders during long deep-space transits, with lack of a visual connection to Earth—even spaceflight can be boring!
- Privacy and habitability challenges
- Increased strain on relationships with family and friends
- Increased risk of feelings of estrangement from ground-support teams
B.3 Assessing medical risks
Given the limited amount of medical equipment that can be brought along, a critical step in planning medical care for deep-space missions is to decide what medical situations to equip and prepare the crew for.
Such decisions are informed by considering medical situations that have arisen in analogous environments, such as in Antarctic research stations and aboard submarines. These situations include strokes, appendicitis, kidney stones, bone fractures, cancer, intracerebral hemorrhage and psychiatric illness.
Statistical models such as NASA's Integrated Medical Model compute the likelihood of the occurrence of various conditions. When aggregated in proportion to the clinical severity of these conditions, this yields an overall medical risk for any given mission profile.
Table 1 categorizes a number of possible deep-space medical conditions, those deemed common and anticipated during a deep-space mission, those that are worse and more rare but still likely and those that are unlikely and more severe but still worth preparing for. One must then make an informed decision to disregard the remaining conditions that are either too unlikely, not treatable with limited medical training or require too many resources to realistically manage. Severe impairment or death of an affected crew member are soberly accepted as potential prognoses. Training in medical ethics and end-of-life care will understandably be part of deep-space crew training.
| Common/Anticipated | Occasional | Rare, but to be prepared for | Not AddressedTable note * |
|---|---|---|---|
|
|
|
|
Overview of medical conditions that have occurred or may occur during spaceflight. Adapted from Barratt and Pool and Watkins.
B.4 Expanding the Role of the Crew Medical Officer
Medical operations in deep space will become more autonomous, as real-time consultation with and intervention by ground-based medical teams will be impossible. In effect, some of the responsibilities currently held by the Flight Surgeon on the ground will devolve to the onboard crew medical officer (CMO). The CMO will therefore need to be a broadly experienced physician, with qualifications in space and emergency medicine as well as some basic surgical training, as there are likely to be cases during a lengthy mission in which surgical intervention is required.
Clinical and procedural skills will require advanced crew training/credentialling, in addition to "just-in-time
" training and simulation during these long flights to retain medical skills. Quantitative methods for performance evaluation and competency-based education models will help ensure focused training on relevant tasks for the mission at hand.
B.5 Onboard Medical Systems for Deep-Space Missions
Onboard medical systems will be more intelligent than healthcare-delivery equipment in any previous spacecraft. Digital information networks will incorporate crew-worn sensors and the monitoring of crew activity such as food and drink intake, sleep and exercise. Onboard computer memory will be at a premium and the capacity for data transmission back to Earth will be limited. Therefore, biomedical data will need to be analyzed on-the-fly by AI-enabled systems, with the raw data discarded. Clinical decision-support systems will assist the CMO to maintain crew health and to diagnose and treat illness.
The size of the onboard medical-care facility will be limited, consisting of compact medical kits with a range of ambulatory, resuscitation and surgical equipment, augmented by 3-D printing of biomedical devices and instruments, and perhaps even in-situ production of pharmaceuticals. Since medical evacuation will not be an option, the onboard medical facility will need to provide complete and definitive care for the range of envisioned conditions.
A deep-space healthcare system provided by Canada might comprise the following:
- Non-invasive vital-signs monitoring, with AI-enabled, real-time data screening
- Compact point-of-care biological sample analyzer ("
lab-on-a-chip
") - Environmental health monitoring system for the spacecraft/habitat
- Polyvalent and lightweight medical imaging, such as AI-assisted ultrasonography
- Medical knowledge database with clinical decision support
- Procedural training/simulation and support with augmented reality visualization
- In-space 3-D medical device manufacturing
- Integrated and automated crew health maintenance and injury prevention program
- Canada-based medical operations control centre, with a broad network of available consultants for telemedicine support, as required
B.6 Other Crew Health-Related Systems
Maintenance of crew health will be essential for mission success. Exercise devices designed to minimize cardiovascular and musculoskeletal deconditioning will by necessity be smaller than the systems currently used aboard the ISS. These could include a virtual-reality component to allow the crew to mentally "escape
" the onboard setting during exercise.
Radiation shielding material will be integrated into the structure of the spacecraft to protect the crew from ionizing radiation. This will also include a safe-haven to shelter the crew from high doses of radiation in a major solar flare.
Crews will need to be less reliant on cargo replenishment. Given the distance from Earth, resupply of the spacecraft or habitat with consumables such as water, air, food and clothing, as well as replacement mechanical parts, will be limited or impossible. Spacecraft systems will thus need to be reliable, robust and function autonomously. The crew will also need to be able to maintain and repair them, with limited monitoring and management by flight-controllers on the ground. Life-support systems, for example for the revitalization of cabin air, recovery of wastewater and collection and processing of human waste, will need to be near-closed-loop and more robust and reliable than those aboard current spacecraft. Future habitats may be outfitted with horticultural modules to supplement these life-support systems and provide fresh food.
Environmental monitoring of the spacecraft habitat, for instance the cabin atmosphere, water quality and sound levels, will no longer rely on the return of air and water samples to the ground for analysis. Instead, such monitoring will require onboard analysis by crew members, who will be trained to identify contaminating microbial organisms.
Appendix C Terms of Reference – Advisory Council on Deep-Space Healthcare
In this section
Background
In , the Canadian Space Agency (CSA or the Agency) established a task force of Canadian healthcare professionals known as the Expert Group on the Potential Canadian Healthcare and Biomedical Roles for Deep-Space Human Spaceflight to consider a possible role for Canada in astronaut healthcare and performance during deep-space missions. This Expert Group, with membership external to the CSA, was asked to recommend to the CSA a role that would be critical, visible, scalable, affordable and socially beneficial to Canadians, and that would build on our country's reputation as a respected leader among spacefaring nations.
Following five months of deliberations, the Expert Group reported its findings to the president of the CSA. Its overall counsel was that the Agency and a partnership of national stakeholders should pursue leadership in deep-space astronaut healthcare prior to the Mars exploration missions. The Expert Group presented four recommendations, the final of which proposed that:
To assist the Canadian Space Agency with development and implementation of this potential opportunity, an external and diverse collaborative body should be established, representing Canada's space operational, health service delivery, commercial, research and government expertise.
These terms of reference define the functions of the "external and diverse collaborative body
" mentioned in this fourth recommendation. Known as the Advisory Council on Deep-Space Healthcare and reporting to president of the Agency, this body builds upon the work of the Expert Group and advances the definition of a possible role for Canada in astronaut healthcare and performance during deep-space missions.
Mandate
The Advisory Council on Deep-Space Healthcare ("Advisory Council
" or "Council
") will assist the CSA as it endeavors to define in detail a potential deep-space healthcare program for Canada that is nationally critical, visible, scalable, affordable and socially beneficial. The Advisory Council will recommend the vision, mission and values of the program and identify aligned national stakeholders.
Responsibilities
Whereas the Expert Group answered the "what
" and "why
" questions of a potential deep-space healthcare initiative for Canada, the Advisory Council will answer the "how
" and "who
" questions.
Specific tasks of the Advisory Council include:
1. Provide Recommendations
In consultation with the CSA and other experts, the Advisory Council will provide recommendations on how to define a multi-partner national program in astronaut healthcare and performance. More specifically, the Advisory Council will:
- Recommend priority areas to be considered for the potential deep-space healthcare program for Canada
- Identify potential national stakeholders with mandates and priorities aligned with those of the deep-space healthcare program for Canada and the Agency, and propose an organizational structure for a multi-stakeholder partnership
- Facilitate the CSA's engagement with the Canadian healthcare, biomedical, science, performance, Indigenous and governmental communities and their relevant members
- Identify and articulate ideas and concepts that could be presented to these communities to collectively define a potential Canadian role in deep-space healthcare
- Conceptually design the multi-stakeholder partnership ecosystem and its interdependencies with other national and international partners
- Identify relevant stakeholder resources and define the potential nature of their contributions (functional, financial, in-kind)
- Identify other key stakeholders external to the deep-space healthcare program
2. Provide Expert Opinion
As national leaders of healthcare, members of the Advisory Council will provide the Agency with expert opinion on the clinical, technical, scientific, programmatic and social aspects of a deep-space healthcare initiative. They will also provide their opinion on innovation and knowledge-translation plans and investment priorities.
3. Participate in the Development of National Awareness
The Advisory Council will support the CSA in developing the vision, objectives and excitement of a potential Canadian role in deep-space healthcare to be communicated by the CSA to key stakeholders, decision-makers, media and the public.
Responsibilities of the Advisory Council do not Include:
- Detailed costing/budgeting of the potential deep-space healthcare program for Canada
- Acting as representatives of the CSA or in the CSA's name, including but not limited to discussing, engaging in, negotiating or concluding agreements or arrangements of any kind with any third party
- Engaging with potential partners and negotiating a Canadian role in deep-space healthcare
- Communicating to anyone the CSA's vision and objectives
These responsibilities are those of the Canadian Space Agency.
Membership
Individual members of the Council are chosen because of their status as experts and their demonstration of leadership within their professional communities. They are experienced, influential and well-networked individuals with the ability to facilitate the CSA's engagement with potential stakeholders at the highest levels. Collectively, the skills, knowledge and experience of the Advisory Council members will contribute to the group's mandate and tasks.
Participation in the Advisory Council is agreed to by each member on a voluntary basis.
The membership will represent diversity (gender, regions, ethnicity, age) and expertise in clinical, public health, research, technology, government, commercial, space operational matters and Indigenous affairs.
The Advisory Council will consist of members from, but not limited to, these space and healthcare sectors:
- Former astronauts and other space industry
- Healthcare innovation industry and institutions
- Aligned research institutions (e.g., NRC, CIHR)
- Aligned health practitioner organizations (e.g., CMA, Society of Rural Physicians of Canada, Indigenous health experts)
- Allied federal government departments (e.g., ISED, HC, FNIHB)
- One international member (NASA)
Membership excludes individuals, organizations and special-interest groups that might have conflicting or vested interests in an ultimate program or present a risk, potential risk or perceived risk of conflict of interest.
Advisory Council membership also includes three ex-officio positions:
- Flight Surgeon, CSA
- Director General, Policy, CSA
- Director General, Space Exploration, CSA
Duration
The Advisory Council will deliver its report and recommendations to the president of the Canadian Space Agency. Ultimately, it is the responsibility of the CSA and the Government of Canada to decide on any potential role for Canada in human exploration of space beyond the ISS.
The Advisory Council will remain in place until , or until such time as the CSA deems it has fulfilled its mandate.
Appendix D Advisory Council Member Biographies
Dr. Robert Thirsk (Chair)
Retired Astronaut, Canadian Space Agency
Dr. Robert Thirsk received degrees in Mechanical Engineering from the University of Calgary and from the Massachusetts Institute of Technology (MIT). He also holds a Doctorate of Medicine from McGill University and an MBA from the MIT Sloan School of Management.
Bob has flown on two space missions as a member of the Canadian Space Agency's astronaut corps. He first flew aboard the space shuttle Columbia in with six international crewmates as part of the Life and Microgravity Spacelab Mission. This 17-day mission was devoted to the study of life and materials sciences.
In , Bob launched aboard a Russian Soyuz spacecraft to the International Space Station (ISS). As members of the ISS Expedition 20/21 crew, Bob and his five crewmates performed multidisciplinary research that has brought about terrestrial benefit and enabled future space exploration. During the 188-day expedition, the Expedition 20/21 crew also performed robotic operations and maintenance of station systems and payloads. Bob is a strong promoter of an economy based upon exploration and innovation. He encourages students to build their career dreams upon a solid educational foundation and advanced skills.
Diane Côté
CEO, MEDTEQ+
Industrial Research and Innovation Consortium
Diane Côté is CEO of MEDTEQ+, whose mission is to accelerate the development of innovative healthcare solutions through collaborative projects involving teams of industrial, academic and clinical partners. She is a member of the Executive Committee of the Digital Health and Discovery Platform (DHDP) led by Imagia and the Terry Fox Research Institute. She is also a member of the Advisory Council on Deep-Space Healthcare of the Canadian Space Agency.
Diane was Vice-President of the Board of Directors of the Fonds de Recherche du Québec - Santé (FRQ-S). She has been a member of the Life Sciences Advisory Group of Global Affairs Canada and was a member of the Board of AlterGo, a non-profit organisation supporting social inclusion of people with functional disabilities. Diane was previously Vice-President - Quebec of Medtech Canada, the national association created by and for the Canadian medtech industry. During her work in industry, she was CEO of a healthcare technology company specializing in AI/neural networks for clinical risk management tools. She held various management assignments at IBM Canada. She also led mandates in strategic planning, financing and partnerships at Innovitech, a strategic broker in the development of innovative economic and business models.
Dr. Valérie Gideon
Associate Deputy Minister, Indigenous Services Canada
Dr. Valérie Gideon is a member of the Mi'kmaq Nation of Gesgapegiag, Quebec, and a proud mother of two young girls.
She currently holds the position of Associate Deputy Minister of Indigenous Services Canada. From -, she was the Senior Assistant Deputy Minister, First Nations and Inuit Health Branch (FNIHB), Indigenous Services Canada. From -, Valerie held the position of Assistant Deputy Minister, Regional Operations, Health Canada. From -, she was Director General, Strategic Policy, Planning and Analysis at FNIHB. From -, she held the position of Regional Director for First Nations and Inuit Health, Ontario Region, Health Canada.
Prior to working at Health Canada, Valérie's experience consisted mainly of working in First Nations health advocacy as Senior Director of Health and Social Development at the Assembly of First Nations and Director of the First Nations Centre at the National Aboriginal Health Organization. She was named Chair of the Aboriginal Peoples' Health Research Peer Review Committee of the Canadian Institutes of Health Research in .
Valérie graduated from McGill University (Montreal) in with a Doctorate degree (Dean's List) in Communications (dissertation pertaining to telehealth and citizen empowerment). She previously completed a Master of Arts in at McGill. She is a founding member of the Canadian Society of Telehealth and former board member of the National Capital Region YMCA/YWCA.
Dr. Rick Glazier
Scientific Director, Institute of Health Services and Policy Research, CIHR
Dr. Rick Glazier is Scientific Director of the Institute of Health Services and Policy Research at the Canadian Institutes of Health Research (CIHR). He is also a senior core scientist at ICES, a staff family physician and scientist in the MAP Centre for Urban Health Solutions at St. Michael's Hospital in Toronto, and a professor at the University of Toronto, Faculty of Medicine, Department of Family and Community Medicine, and the Dalla Lana School of Public Health. He is author of more than 300 publications in peer-reviewed journals and has been named one of the top 20 pioneers in family medicine research by the College of Family Physicians of Canada. From to he was the scientific program lead for Primary Care and Population Health at ICES.
Rick's research interests include evaluating health system transformation, primary care health services delivery models, health of disadvantaged populations, management of chronic conditions, and population-based and geographic methods for improving equity in health.
He earned his medical degree at Western University and completed his family medicine residency at Queen's University. He received a Master of Public Health degree at Johns Hopkins University and completed a residency in General Preventive Medicine and Public Health through Johns Hopkins and the World Health Organization.
Jas Jaaj
Managing Partner, Deloitte
As Managing Partner, AI and Data (including Omnia AI), Jas oversees a globally recognized team at Deloitte of artificial intelligence strategists, data scientists, machine learning engineers, data engineers, and risk specialists, working to help businesses drive significant growth through innovation, technology and data-driven decision-making. He also champions the firm's acceleration to be an AI-first enterprise, collaborating with business leaders across Audit, Tax, Risk Advisory, Financial Advisory and Consulting to infuse AI and a data-informed approach into all key market offerings to bring differentiated value to our client's transformation journey.
With more than 20 years of experience in tech, data and AI, Jas has been with Deloitte for 13 years, specializing in collaborating with large enterprises to transform their organizations from being AI-aware to AI-first. Prior to joining Deloitte and in previous roles within the firm, Jas has had a stellar track record of being an innovative leader, having led multiple practices in the emerging technology space, including Blockchain and Digital.
Jas is passionate about fueling the Canadian economy by leveraging the power of AI. He is a change agent and an active advisor to multiple external boards and the AI start-up ecosystem.
Dr. Deepak Kaura
Chief Medical Officer, 1Qbit
Dr. Deepak Kaura is a pediatric radiologist and Chief Medical Officer of 1QBit, a Vancouver-based quantum computing software company. As a leader in the industry, he has built health enterprise partnerships for data, developing and clinically validating several machine learning products for radiology, and working with Health Canada to develop and refine regulations for machine learning tools in health. He is also the Vice-Chair of CAN Health Network.
Prior to these appointments, Deepak was chair of the board of Joule, a Canadian Medical Association subsidiary. He also spent five years in Qatar with the Sidra Medical and Research Center, most recently as Executive Chairman of the Foundational Clinical Services Management Group, where he helped to set new standards in patient care for women and children and led ground-breaking work in the application of machine learning to healthcare. Deepak has also served several medical and scientific societies, including the Royal College of Physicians and Surgeons of Canada as a Subspecialty Chair in Pediatric Radiology.
He received his MBA from HEC Paris, FRCPC following training in Calgary and his MD from the University of Manitoba. He has held faculty appointments as Associate Professor at Cornell University and the University of Calgary.
Gilles Leclerc (Ex-Officio Member)
Director General, Space Exploration, CSA
Gilles Leclerc joined the Canadian Space Agency (CSA) in . He gained experience in space policy and program management in a variety of national and international technology development, satellite communications, Earth observation and flight simulation projects.
Between and , Gilles was posted at the Canadian Embassy in Paris as Counsellor for Science, Technology and Space Affairs and Canada's Delegate to the European Space Agency. He became Director, Technology Management and Applications and in , Director General, Space Technologies.
Since , Gilles is Director General, Space Exploration, leading the Agency's human and robotic exploration activities, including Canada's participation in the International Space Station; Astronomy and Planetary missions; Human Spaceflight (Canadian Astronauts); Health Sciences; and Space Medicine.
In and , Gilles served as Acting President and Vice President of the CSA. He is Canada's representative on the International Space Station and Gateway Multilateral Control Boards, and he currently chairs the International Space Exploration Coordination Group, a forum of 26 space agencies.
He studied Engineering Physics and Applied Geophysics at Université Laval and McGill University.
Dr. Keith MacLellan
Co-founder, Society of Rural Physicians of Canada
Dr. Keith MacLellan received a Bachelor of Arts in History, a Bachelor of Science in Molecular Biology and an MDCM in Medicine at McGill University. After a rotating internship in St. John's, NL, he worked as a rural/remote general practitioner in Northern Newfoundland and Labrador and in other rural and remote areas of Canada. He has been a general practitioner in Shawville, QC, for more than 35 years, where he practices a broad range of medical, intensive-care and surgical skills, as well as research and teaching.
Keith is co-founder of the Society of Rural Physicians of Canada, now with more than rural/remote members. He established the Annual National Conference on Rural and Remote Medicine and the national Rural Critical Care Course, committing to Canadian and global medical skills training for rural/remote physicians. He is active nationally and internationally in political advocacy for equitable healthcare for rural/remote communities, supported by numerous educational and policy publications. His interests are access to specialty care by rural/remote communities and the fundamentals of medical generalism. He is an Assistant Professor of Family Medicine at McGill and was named a member of the Order of Canada in .
Dr. Paul McBeth
Clinical Associate Professor of Surgery and Critical Care Medicine, University of Calgary
Dr. Paul McBeth is a Clinical Associate Professor in the departments of Surgery and Critical Care Medicine at the University of Calgary. He began his career as an engineer with post-graduate training in surgical robotics and human performance evaluation. He was lead clinical engineer in the design and development of Project neuroArm, an image-guided neurosurgical robot system based on technologies developed for the Canadarm.
Paul completed post graduate training in General Surgery at the University of Calgary, with sub-specialty training in Critical Care Medicine at the University of British Columbia and Trauma Surgery at the Elvis Presley Memorial Trauma Centre in Memphis, Tennessee. During his medical training, he continued his research interests in surgical robotics, remote ultrasound and aerospace medicine. He is also an adjunct professor at the Schulich School of Engineering, where he is involved in several technology-development projects.
Paul has been conducting research in the field of acute-care surgery and robotics for the past 15 years, having published more than 150 journal articles, conference papers, abstracts and patents in this field. He is currently leading a research program supporting intelligent systems monitoring for pre-hospital transport of critically ill patients. He is also a recognized leader in medical/surgical education.
Dr. Alex Mihailidis
Barbara G. Stymiest Research Chair in Rehabilitation Technology,
University of Toronto and Toronto Rehab Institute
Scientific Director, AGE-WELL Network of Centres of Excellence
Dr. Alex Mihailidis is Associate Vice-President for International Partnerships at the University of Toronto and Scientific Director of the AGE-WELL Network of Centres of Excellence, which focuses on the development of new technologies and services for older adults. He is a professor in the Department of Occupational Science and Occupational Therapy (U of T) and in Biomedical Engineering (U of T), with a cross appointment in the Department of Computer Science (U of T).
Alex has been conducting research in the field of technology to support older adults for the past 17 years, having published more than 200 journal papers, conference papers and abstracts in this field. He is also very active in the rehabilitation engineering profession, as the past-president of Rehabilitation Engineering and Assistive Technology Society of North America (RESNA). He was named a Fellow of RESNA in , which is one of the highest honours within this field of research and practice.
Alex received a B.A.Sc. in Mechanical Engineering from University of Toronto in , an MASc in Biomedical Engineering in from the University of Toronto and a PhD in Bioengineering (Rehabilitation Engineering) in from the University of Strathclyde (Glasgow, Scotland).
Mary Preville (Ex-Officio Member)
Vice President, Space Program Policy, Canadian Space Agency
Mary Preville joined the Canadian Space Agency in . She is currently Vice-President, Space Program Policy, responsible for policy, planning, international and business relations, and communications and public affairs.
Previously, Mary was Director General of Earth Sciences at Natural Resources Canada, where she was responsible for Arctic logistics in support of scientific advancement, the Climate Change Impacts and Adaptation program, as well as for a number of international and policy issues. For many years, she was the lead executive responsible for energy research and development programs, and she spent two years at the International Energy Agency in Paris.
Mary holds a Bachelor of Science (Chemistry) from McGill University and a Master of Business Administration from the University of Ottawa.
Dr. Rob Riddell (Ex-Officio Member)
Flight Surgeon, Canadian Space Agency
Dr. Rob Riddell joined the Canadian Space Agency in . He was Deputy Crew Surgeon for Astronaut David Saint-Jacques' mission to the ISS in /. He is currently medical lead for the CSA's Deep-Space Exploration Healthcare efforts.
When he joined the CSA, Maj (Ret'd) Riddell was serving as the Senior Medical Officer at Joint Task Force 2 (JTF-2), Canada's Counter-terrorism unit in the Canadian Armed Forces. Prior to embarking on his medical career, Bob served as an infantry and special operations officer in the Canadian Armed Forces, including five years as an Assaulter Officer in JTF-2. He had several overseas operational experiences in Bosnia, Afghanistan and Iraq. His service with JTF-2 during the Afghanistan campaign in earned him the Meritorious Service Medal from the Governor General of Canada.
Bob received his Bachelor of Chemical Engineering at the Royal Military College in . He earned his medical degree from Dalhousie University, followed by a Rural Family Residency through the University of Alberta. Clinically, he continues to work part-time as an emergency-room physician in rural communities in Ontario and for Project Trauma Support, an organization for military members, veterans and first-responders who suffer from moral injury and PTSD. He is also the lead for Prevail, a new virtual healthcare program that supports members of the Canadian Special Operations Forces during their transition from military to civilian life.
Dr. David Saint-Jacques
Astronaut, Canadian Space Agency
Dr. David Saint-Jacques is a Canadian astronaut with the Canadian Space Agency (CSA). He is also an astrophysicist, engineer, physician and pilot.
Born in Quebec City, David has always been keen to explore the world around him. Prior to joining the Canadian Space Program, he practised family medicine in various Canadian northern communities overlooking Hudson Bay. Before that, he worked as an astrophysicist in observatories around the world.
David was selected by the Canadian Space Agency in , and moved to Houston as a member of the 20th NASA astronaut class. Upon completion of basic training, he worked as Capcom (the liaison between the team on the ground and the crew in space) and carried out various operations, planning and support functions for NASA's Mission Control Center and Astronaut Office.
On , David flew as co-pilot of a Soyuz rocket to the International Space Station, where he stayed 204 days as a member of Expedition 58/59, the longest Canadian space mission to date. He conducted a suite of Canadian and international scientific experiments. He became the fourth CSA astronaut to conduct a spacewalk and the first CSA astronaut to use Canadarm2 to catch a visiting spacecraft.
Dr. Terrance Taddeo (Observer Status)
Chief Medical Officer, JSC NASA
Dr. Terrance A. Taddeo is the Chief Medical Officer at NASA's Johnson Space Center, a position he assumed in . In this role, Terrance leads a team of experienced space-medicine physicians in managing the health risks related to human spaceflight, provides health and medical technical oversight to NASA human spaceflight programs, and leads occupational health implementation for the Center.
Terrance began his career in as a Flight Surgeon in the JSC Medical Operations Branch. For 15 years he served as an operational Flight Surgeon, supporting the NASA/Mir missions, the Space Shuttle program and the International Space Station program.
He serves in several leadership roles in the multinational medical framework established for the ISS program, including his current role as Co-Chair of the Multilateral Space Medicine Board, and Alternate Chair of the Multilateral Medical Policy Board.
From to , Terrance supported the mission of the United States Air Force Reserve as a Flight Surgeon. He is a recipient of the NASA Exceptional Service Medal and the NASA Exceptional Leadership Medal. He is a Fellow of the Aerospace Medical Association and a member of the American Society of Aerospace Medicine Specialists.
Gail Turner
Former Director of Health Services, Nunatsiavut Government, Northern Labrador
Gail Turner is Inuit, a beneficiary of the Labrador Inuit Land Claim, who retired in from the position of Director of Health Services of the Nunatsiavut Government, Northern Labrador. She holds a Bachelor of Nursing degree from Memorial University of Newfoundland, a Master of Adult Education from St. Francis Xavier University and holds many additional certificates in health and administration through distance programs. Her early career was spent in acute-care nursing in Ontario and the United Kingdom.
For the last twenty-six years Gail has been working in Labrador with Inuit, Southern Inuit of NunatuKavut, settlers, First Nations. Since , she has worked exclusively with the Inuit. She has presented on Inuit health at provincial, regional, national and international meetings and symposiums, including the World Cancer Congress in . She is passionate about the North and the need for First Nations, Inuit and Métis to be heard and truly engaged in the planning of their healthcare. She is currently Inuit Advisor to the Canadian Partnership Against Cancer (CPAC).
Gail is a recent recipient of the Labradorians of Distinction Award for services to health and community. As a senior, she has a growing interest in senior wellness, access to appropriate home care, long-term care and aging in place.
Appendix E The Expert Group on the Potential Canadian Healthcare and Biomedical Roles for Deep-Space Human Spaceflight
Created in , with membership entirely external to the Canadian Space Agency, the Expert Group on the Potential Canadian Healthcare and Biomedical Roles for Deep-Space Human Spaceflight (Expert Group) was tasked with advising the CSA president on a possible Canadian contribution to the next steps in international space exploration. It met eight times between and , in consultation with health, space and innovation leaders, as well as international experts.
In , the Expert Group published its report Canadian Healthcare in Deep Space: Advancing our country's leadership in autonomous care in space and on Earth.
The overall counsel of the Expert Group was that the CSA, along with aligned national partners, is well positioned to secure a role in the coming years as an international leader in deep-space astronaut healthcare, tackling at the same time some of the most pressing needs of Canada's national healthcare system. The Canadian health innovation ecosystem has the required depth, breadth and credibility as well as the expertise, resources and ambitions. As no spacefaring nation has prior experience with deep-space healthcare, there is an opportunity to develop this emerging field as a new niche area of space competence.
Herewith a summary of the report:
- Part 1, The Space Exploration Roadmap, reviews the status (in ) of the envisaged plans for international exploration of deep space.
- Part 2, Crew Health and Performance Issues of Deep-Space Missions, describes the anticipated medical challenges of this new class of mission and explains the need to rethink the model of astronaut healthcare delivery to be more autonomous, patient-centric and point-of-care. An argument is also made for the opportunity to develop and validate these technologies for use on Earth first, to the benefit of society.
- Part 3, Canadian Strengths in Healthcare and Performance, highlights those areas where we perform well. They include research skills and talent, health research and clinical leadership, healthcare innovations, including diagnostic products, medical robotics, training and simulation, and technology trends, in particular artificial intelligence.
- Part 4, Socioeconomic Yardsticks that Should be Moved, presents the challenges faced by the Canadian healthcare system in terms of an urgency for modernization and innovation in the organization and delivery of care, the growing needs of an aging population, and the moral imperative to improve accessibility and equity for all, from urban chronic-care patients to rural and remote populations, in particular Indigenous communities.
The report makes the following recommendations:
Recommendation #1
Canada should invest significantly in deep-space autonomous healthcare, as a bold contribution to space exploration and a means to develop national capacity in virtual healthcare for the benefit of all Canadians.
Approaches, training and technologies developed for space could be transformative in the delivery of national healthcare and strengthen the stated Canada Health Act () principles of universality and accessibility.
Recommendation #2
Canada should pursue a role as the lead integrator and operator for astronaut healthcare in deep-space missions.
Canada's goal should be leadership in deep-space astronaut healthcare, not merely a contributor role. This would include oversight of in-space medical operations on behalf of international partners. Ground-based responsibilities would focus on integration and training. In particular, the Expert Group envisioned a network of Northern Demonstration Sites, testbeds in which technologies intended for deep-space are validated by remote-community practitioners and patients.
Recommendation #3
In addition to operational oversight, Canada should contribute healthcare technologies to the deep-space healthcare facilities, according to our national expertise.
Canadian industry has the capability and capacity to contribute sub-systems to the onboard crew healthcare system, such as monitoring and diagnostics; surgical robotics; medical imaging and analysis; and simulation-based training.
Recommendation #4
To assist the Canadian Space Agency with development and implementation of this potential opportunity, an external and diverse collaborative body should be established, representing Canada's space operational, health service delivery, commercial, research and government expertise.
A deep-space healthcare initiative is beyond the current mandate, expertise and resources of the CSA. However, it is not beyond the capabilities of an integrated partnership of Canadian space, healthcare and technology players. This partnership would also prioritize the inclusion of Indigenous communities as early, full and active partners.
Appendix F Briefings to the Advisory Council by Subject-Matter Experts
Guided by an ambitious work plan, the Advisory Council on Deep-Space Healthcare benefitted from hearing a number of subject-matter experts speak on a broad range of topics. The diverse topics covered and perspectives shared have enabled us to provide informed advice about the foundational elements of a potential Canadian deep-space healthcare initiative.
The following is a list of the briefings received from expert presenters over the course of our mandate, in chronological order:
Overview of Space Exploration
Gilles Leclerc (Director General, Space Exploration, Canadian Space Agency)
Briefing outlined global deep-space exploration plans and the Lunar Gateway and Artemis rollout plans.
Low-Earth Orbit Model of Healthcare Delivery
Dr. Raffi Kuyumjian (Flight Surgeon, Canadian Space Agency)
Overview of the current "
Earth-reliant
" model of healthcare delivery in space, including the ISS medical infrastructure and inflight medical support.Indigenous Healthcare in Canada
Dr. Evan Adams (Chief Medical Officer, BC First Nations Health Authority)
An overview of the perspectives and challenges associated with the delivery of healthcare to Indigenous communities in Canada.
Deep-Space Healthcare Model
Dr. Robert Riddell (Flight Surgeon, Canadian Space Agency)
An overview of the operational context of deep-space exploration and its inherent healthcare challenges, including distance-from-Earth, communications, resupply logistics and medical evacuation.
Remote Medicine in Canada and Beyond
Dr. James Rourke (Memorial University of Newfoundland)
Outline of rural and remote healthcare in Canada, including the challenges associated with delivering specialized care by non-specialists and the importance that contextual experience plays in healthcare outcomes in rural and remote communities.
Artificial Intelligence (AI) in Healthcare
Dr. Anna Goldenberg (Chair of Biomedical Informatics and Artificial Intelligence, Hospital for Sick Children in Toronto)
An overview on the advances and challenges of AI in healthcare and AI's potential role in the delivery of healthcare in deep space and remote regions.
Remote Surgery in Space
Dr. Garnette Sutherland (Project neuroArm, University of Calgary)
An overview of surgical approaches and operational constraints to performing surgery in space as well as current surgical capabilities and anticipated innovations, in particular robotic surgery, with potential for space applications.
Remote Surgery in Canada
Dr. Mehran Anvari (Centre for Surgical Invention & Innovation, McMaster University)
An overview of the surgical approaches and operational constraints to performing surgery in remote terrestrial sites, current surgical capabilities and anticipated innovations in this field in Canada.
Canada's Digital Technology Supercluster and the Secure Health and Genomics Platform (Aspen): A Case Study of a Healthcare Innovation Partnership
Ms. Joyce Drohan and Mr. Niraj Dalmia (Deloitte Canada)
An overview of Canada's Digital Technology Supercluster and of Aspen, the Secure Health and Genomics platform and shared insights in building and operating a complex ecosystem.
The Alaskan Example: An Innovative Community-Based Approach to Delivery of Primary Healthcare
Ms. Gail Turner (Retired Nurse and former Director, Health Services, Nunatsiavut Government, Northern Labrador)
An overview of an exemplary Alaskan remote healthcare delivery model that engages local community members in the management and delivery of care in their communities.
Rural Generalist Medicine and Specialist Training for Remotely located Physicians
Dr. Stuart Iglesias (Society of Rural Physicians of Canada)
Presentation on rural generalist medicine in Canada and specialist training for remote physicians, including surgery skills and anesthesia, and its applicability to deep-space contexts.
Training of Healthcare Practitioners
Dr. Andrew Padmos (Royal College of Physicians and Surgeons of Canada)
A review of the current paradigm in the training of specialist physicians by the Royal College, including competency-based training and certification.
Industry Perspectives of a Deep-Space Healthcare Partnership
Ms. Diane Côté (CEO, MEDTEQ+)
An outline of the priorities, drivers and challenges of the health technology industry.
The Future of Training
Ms. Rekha Ranganathan (President, CAE Healthcare)
Presentation on simulation and technology-enabled training and its potential to make healthcare-delivery safer.
The Pan-Canadian AI Strategy and AI-for-Health
Dr. Elissa Strome (AVP Research, CIFAR)
Presentation on the findings of the task force on AI for Health (AI4H) Strategy.
Coordinated Accessible National (CAN) Health Network
Dr. Deepak Kaura (Chief Medical Officer, 1QBit)
An overview of the CAN Health Network, a collaboration between the federal government and industry, to assist Canadian health technology companies unlock their economic potential.
Engaging with First Nations, Inuit and Métis
Ms. Andrea Reed (VP Strategic Partnerships, Canadian Partnership Against Cancer) & Ms. Nicole Robinson (Manager, Canadian Partnership Against Cancer)
An overview of the - Canadian Strategy for Cancer Control, the development of which was guided by First Nations, Inuit and Métis partners.
A Primer on Artificial Intelligence in Healthcare
Dr. Deepak Kaura (Chief Medical Officer, 1QBit) and Mr. Jas Jaaj (Managing Partner, Deloitte Canada)
An overview of the meaning and impact of AI and related concepts, as well as their influence on the future direction of healthcare technology.
Lunar Surface Exploration Scenarios
Dr. Christian Lange (Head, Space Exploration Strategic Planning, Canadian Space Agency)
Current architecture and timelines for lunar surface and Gateway missions. Implications of the updated mission scenarios on crew healthcare planning and international partner roles.
-
Exploration Healthcare - Artemis
Dr. Terry Taddeo, Dr. Sharmi Watkins (Human Health and Performance Directorate, NASA)
An overview of the stressors, impacts and risks of the human system in deep space. The mission strategy and architecture influences on the provision of lunar healthcare.
CSA Food Production Initiative
Dr. Matthew Bamsey (Senior Engineer, Space Exploration Strategic Planning, Canadian Space Agency)
An overview of the newly commenced CSA Food Production Initiative and the activities focussed on the interface between space-based and terrestrial food production systems.
A Northern Demonstration Initiative
Dr. Robert Riddell (Flight Surgeon, Canadian Space Agency)
An overview of the Northern Demonstration Initiative, including objectives, collaboration with the Northern BC working group and the CSA's role in the working group.
Beyond these briefings, Council members shared information on medical innovations and healthcare-delivery models in underserved communities in Canada and abroad, as well as facilitated face-to-face engagements with other subject matter experts and potential stakeholders.
Appendix G Candidate Members of a Canadian Deep-Space Healthcare Partnership
The Advisory Council considered many organizations as candidate members of a nascent deep-space healthcare partnership (our national healthcare ecosystem is agreeably deep and broad.) Based on functions, priorities, timelines and ideal partner attributes, we recommend the following organizations as members of such a Canadian partnership.
Partners in the Short Term ( – )
We recommend the following organizations as founding members of a Canadian deep-space healthcare partnership:
- Canadian Space Agency (partnership leader)
- Indigenous Services Canada (representing government departments)
- CAN Health Network, First Nations Health Authority (representing health-delivery agencies)
- Society of Rural Physicians of Canada (representing frontline healthcare practitioners)
- AGE-WELL (representing research institutions)
- MEDTEQ+ (representing industry)
Canadian Space Agency
With a large staff of skilled scientists, engineers and project managers, the Canadian Space Agency (CSA) has considerable spaceflight expertise. The Agency manages several national facilities for flight qualification, systems integration and mission operations. It has trained many international astronauts and ground-support personnel with Agency-developed curricula, learning tools, simulators and instructors. The CSA's operational space medicine division has provided medical support to several past missions of Canadian astronauts. This division continues to advance medical countermeasures to reduce the adverse effects of the space environment on crew health. The CSA's space life sciences group supports a Canadian research community focused on understanding the biological and physiological adaptations that occur in space.
The CSA would contribute program, policy and operational leadership to a deep-space healthcare partnership. It would oversee development of the Roadmap for Action. In the longer term, the Agency would manage operations, quality-control, timelines and scheduling of program deliverables.
Indigenous Services Canada
Indigenous Services Canada (ISC) works collaboratively with partners to improve access to high-quality services for First Nations, Inuit and Métis. It supports and empowers Indigenous peoples to independently deliver services and address socio-economic conditions in their communities.
Improving health outcomes is one of ISC's five key priorities. Timely access of First Nations and Inuit to health services is critical. ISC works in partnership with First Nations organizations to identify, design and deliver health-service solutions that better meet the needs of their communities. The Clinical and Client Care sector of ISC was developed to meet the primary healthcare needs of remote or isolated First Nations communities where limited or no provincial services are available.
In its budget, the federal government targeted $18 billion over the next five years to improve the quality of life and create new opportunities for Indigenous communities, including a $2.6-billion investment in health.
CAN Health Network
The CAN Health Network is a national response to a recommendation of the Advisory Panel on Healthcare Innovation to strengthen collaboration between industry, researchers and governments. The Network works to build a competitive healthcare innovation market in Canada for homegrown solutions. To do this, it identifies business opportunities, selects the best healthcare companies to capitalize on those opportunities, gives those companies access, insights and support to ensure their product is superior, and then provides a large market to quickly scale their businesses.
The CAN Health Network is supported by the federal government through the Federal Economic Development Agency and Western Economic Diversification Canada. It has worked with Canada's most promising biomedical companies to develop, pilot, scale and commercialize new technologies. It would be a valued partner in the deep-space healthcare initiative, by cross-fertilizing terrestrial and space innovations. It could broaden the reach of the CSA's space life sciences group to relevant stakeholders.
First Nations Health Authority
In , the First Nations Health Authority (FNHA) of British Columbia assumed responsibility for the programs and services formerly handled by Health Canada's First Nations Inuit Health Branch - Pacific Region. It is the first province-wide Indigenous health authority of its kind in Canada.
The FNHA today oversees the design, management, delivery and funding of First Nations health programming in British Columbia. It is led and managed by First Nations leaders. It does not replace the role or services of the BC Ministry of Health and Regional Health Authorities, but rather works to collaborate, coordinate, and integrate respective health programs and services to achieve better health outcomes. Specifically, the FNHA works to close the healthcare gaps that exist between First Nations in BC and the rest of the province's population.
The FNHA serves both the urban and rural First Nations population, which includes 203 communities throughout the province. Community-based services are largely focused on health promotion and disease prevention.
Society of Rural Physicians of Canada
The Society of Rural Physicians of Canada (SRPC) is the national voice of more than rural physician members. Its vision is excellent healthcare close to home for all rural Canadians. It champions rural generalist medical care through education, collaboration, advocacy and research. The SRPC develops and advocates health-delivery mechanisms, supports rural doctors and communities in crisis, promotes and delivers continuing rural medical education, and encourages and facilitates research into rural health issues.
The SRPC is one of the champions of the Rural Road Map for Action, a guiding framework for a coordinated, pan-Canadian approach to rural physician workforce planning and improved access to safe, high-quality rural healthcare.
With the College of Family Physicians of Canada (CFPC) and the Royal College of Physicians and Surgeons of Canada, it promotes the acquisition of enhanced surgical, anesthesia and other specialized skills for rural practitioners.
AGE-WELL
AGE-WELL is part of the federal government's Networks of Centres of Excellence program. It focuses on the development of new technologies and services benefitting older adults and their caregivers by increasing personal safety and security, supporting independent living and enhancing social participation. AGE-WELL addresses these healthy-aging issues with a pan-Canadian network of interdisciplinary researchers, industry, non-profits, government, care providers and end-users. The centre also manages training programs, partnerships, knowledge mobilization and the commercial development of technologies.
The AGE-WELL network harnesses the power of new technologies. For instance, smart homes equipped with sensors and computer vision feed a steady stream of data into AI-enabled systems that detect and manage health conditions. Virtual assistants remind those with memory impairment where they left their eyeglasses or to take their medication. Social robots guide those with dementia through everyday tasks, such as getting dressed and making a cup of tea.
MEDTEQ+
MEDTEQ+ is the Consortium for Industrial Research and Innovation in Medical Technology. It is a national pre-market industry association of healthcare innovators. Its mission is to accelerate innovation and to position Canadian products and services in the world market. MEDTEQ+ is the most financially supportive organization for health technology innovation in Canada, having funded more than 100 projects in theme areas including artificial intelligence, augmented and virtual reality, nanotechnologies, optics-photonics, biomaterials, 3-D printing and robotics.
MEDTEQ+ oversees an ecosystem of 200 member companies, health centres, universities and investors, and works to bring the complementary skills of industrial and academic partners together with those of healthcare providers. It promotes long-term collaboration as a means to achieve better outcomes, trust and opportunities. SMEs are supported through investments, de-risked innovations and strategic alliances.
With MEDTEQ+ facilitation, the CSA could gain access to Canada's growing healthcare innovation ecosystem and leverage the consortium's expertise, capacity and network of collaborators.
Partners to be Added in the Medium and Long Term
Although the future roles and needs of the partnership are impossible to foresee, some of the following organizations would become valued members of an augmented partnership in the medium and longer terms. They would help complete a diverse, resourced and synergistic partnership with international impact.
- Health Canada (representing other government departments)
- Provincial/Territorial Health Authorities (representing health-delivery agencies)
- Canadian Medical Association, Canadian Nurses Association, Association of Faculties of Medicine of Canada, Royal College of Physicians and Surgeons of Canada (representing frontline healthcare practitioners )
- CIFAR, Canada Research Coordinating Committee, U15 (representing research institutions)
- Creative Destruction Lab (representing industry)
- Community elders, Canadian astronauts (representing Indigenous and other user communities)
- NASA medical operations, other international partners (representing international partners in an observer status)
Health Canada
Health Canada is the federal department responsible for helping Canadians maintain and improve their health. To carry out this responsibility, it supports activities that:
- Preserve and modernize Canada's healthcare system
- Enhance and protect the health of Canadians, including monitoring the sale and use of drugs and medical devices across Canada
- Work in partnership with others, including provinces, territories and health organizations, to ensure the needs of all Canadians are met
- Communicate health promotion and disease prevention
Health Canada acts as a regulator, service provider, promoter of innovation and trusted source of information. Its functions include financing organizations to promote innovation across Canada; supporting the delivery of healthcare to First Nations and Inuit; regulating food, health and consumer products; and setting and administering national principles to ensure that quality healthcare is available to all Canadians.
The breadth and depth of Health Canada's expertise, coupled with its healthcare oversight mandate, could help accomplish later-term deep-space healthcare goals.
Provincial/Territorial Health Authorities
In Canada, comprehensive healthcare is provided to most Canadians through multiple regional health authorities. The roles and services of health authorities include:
- Delivery of diverse clinical services with expertise in various areas of care
- Credentialled, licensed staff working within systems of care where quality is monitored, education is provided and competencies are maintained
- Systems of delivery that are being continuously updated
- Established IT systems with appropriate data security and management policies
- Well-developed research functions that can be leveraged
- Close ties with universities for training and research, especially within academic health centres
- Experience in the provision of remote/rural care
- Evaluation and implementation of new innovations
Partnering with progressive-minded health authorities from key regions, especially in the early stages of the deep-space healthcare partnership, could help the CSA navigate the complex health-provider ecosystem. (Note: The Agency's current collaboration with health authorities in British Columbia to advance the Northern Demonstration Initiative is already revealing the benefits of such collaboration.)
Canadian Medical Association
The Canadian Medical Association (CMA) is the largest organization of medical doctors in Canada, with more than 75,000 members (physicians, residents and medical students.) The CMA drives meaningful change in healthcare by engaging in health advocacy, public policy, programs and partnerships. It addresses issues facing the medical profession and works to improve the health of Canadians.
The CMA supports the leadership, innovation and training needs of physicians. It provides resources for physicians to incorporate technology in their practices. CMA Joule, a CMA subsidiary, supports physician-led innovation and encourages adoption of knowledge products and innovative technologies and services by physicians. CMA Joule has considerable financial resources.
Assistance in navigating through fragmented regulatory considerations for emerging health and medical technologies would be of particular benefit to a deep-space healthcare partnership. The CMA could also help with policy and training issues and mobilize medical expertise to develop a national roadmap for deep-space healthcare.
Canadian Nurses Association
The Canadian Nurses Association (CNA) is the national voice of 139,000 nurses across all 13 provinces and territories. It provides nationally recognized RN certifications in 21 practice specialties, and delivers professional-development programs as a means to advance nursing excellence and positive health outcomes.
The CNA promotes policy and regulation in the public interest and has influence with national decision-makers. Its report Vision: Improving Long-term Care for People in Canada called for action in response to the effects of the COVID-19 crisis on our health-care system, economy and lives. In particular, it calls for a redesign of long-term care to maximize the safety, comfort, dignity and health of residents.
In , the CNA and associated nursing organizations committed to action against racism with the release of a declaration against anti-Indigenous racism in nursing and healthcare. These same groups are to convene the first National Summit on Racism in Nursing and Health Care later in .
Association of Faculties of Medicine of Canada
The Association of Faculties of Medicine of Canada (AFMC) is a partnership of Canada's 17 faculties of medicine and the voice of academic medicine in Canada. The member faculties graduate 2,700 MDs and undertake $3 billion of biomedical and healthcare research annually. The AFMC serves as an important resource to decision-makers in this country, ensuring research, medical education and clinical care issues are high on the federal government's agenda.
As part of its social accountability mandate, the AFMC strives to improve the health and well-being of Indigenous peoples by training more Indigenous health professionals and by developing safe working and learning environments for learners, faculty and staff. The AFMC works with medical schools on physician resource planning, striving for a physician workforce that is responsive to the health needs of Canadians.
The Future of Medical Education in Canada suite of AFMC projects focus on enhancements to physician education, healthcare delivery and, ultimately, the health of all Canadians.
Royal College of Physicians and Surgeons of Canada
The Royal College of Physicians and Surgeons of Canada (Royal College) is an association of 44,000 physicians that sets national standards for the medical education of specialists in Canada and continuing professional development. This regulatory authority ensures that the training and evaluation of medical and surgical specialists in 80 specialties maintains certain standards of quality.
In , the Royal College commissioned the Task Force on Artificial Intelligence and Emerging Digital Technologies to help the medical profession in Canada prepare for the changes that AI and digital technologies will bring to residency training and the delivery of care.
The Royal College joined forces with the CMA and CFPC in to form the Virtual Care Task Force. It identified the regulatory and administrative changes needed to support virtual care in Canada, and to allow physicians to deliver care to patients across provincial/territorial boundaries.
CIFAR
Artificial Intelligence research is an undisputed core competence of Canada. Our three national AI Institutes—Amii in Edmonton, Mila in Montreal and the Vector Institute in Toronto—are internationally renowned.
In , the Government of Canada appointed CIFAR (formerly the Canadian Institute for Advanced Research) to develop and lead the $125-million Pan-Canadian Artificial Intelligence Strategy. This strategy has enabled these three AI institutes, as well as universities, hospitals and organizations across the country, to attract and retain top research talent.
In , CIFAR established the Task Force on Artificial Intelligence for Health. Following national consultations and deliberations, it published its findings in in its report Building a Learning Health System for Canadians.
The federal budget renewed the Pan-Canadian Artificial Intelligence Strategy with a further $444-million commitment over 10 years. One of the four pillars of its updated strategy is "AI for health
".
Canada's AI research leadership and government investment are strengths upon which to develop a digital-healthcare infrastructure for deep space.
Canada Research Coordinating Committee
The Canada Research Coordinating Committee (CRCC) advances federal research priorities and coordinates policies and programs of Canada's federal research funding agencies and the Canada Foundation for Innovation (CFI). It is a senior strategic forum for initiatives that strengthen Canada's research enterprise, foster world-leading research and advance the socioeconomic well-being of Canadians.
The CRCC comprises the executive heads of the CFI, the Canadian Institutes of Health Research, the Natural Sciences and Engineering Research Council of Canada and the Social Sciences and Humanities Research Council of Canada, as well as the deputy ministers of Innovation, Science and Economic Development Canada and Health Canada, the president of the National Research Council of Canada and the chief science advisor.
Of particular note to deep-space healthcare, the CRCC oversees the New Frontiers in Research Fund. It is investing $275 million over the five-year period beginning in fiscal -, and $124 million annually thereafter, to support international, interdisciplinary, fast-breaking and high-risk/high-reward research.
U15
The U15 is a collective of Canada's most research-intensive universities. They foster the development and delivery of long-term, sustainable higher education and research policy, both in Canada and around the world.
The U15's role is to foster a research environment where universities can continue to drive ground-breaking research. Canada's U15 institutions undertake fundamental research, train tomorrow's citizens, entrepreneurs and leaders, and work with partners from the public and private sectors to mobilize and capitalize on knowledge. They influence the national policy agenda and provide critical advice about higher education, research and development.
Top-quality university research is the foundation of our innovation ecosystem, which is one of Canada's core competitive advantages. U15 universities strengthen Canada's economy and attract talented students and faculty. Member institutions undertake 80% of all competitive university research in Canada, conduct $8.5 billion of research annually and contribute more than $36 billion each year to the national economy.
Creative Destruction Lab
The Creative Destruction Lab (CDL) is a not-for-profit organization that offers mentorship by entrepreneurs and angel investors to science and technology-based start-ups. The program provides advice on technology roadmaps, business-development support and opportunities to raise capital. It operates 10 locations globally, including five sites in Canada.
The CDL has 16 streams, including one specifically for space and one for health. The space stream brings together mentors from fields related to space exploration and development. This stream is tailored toward early-stage companies that are applying AI and other advanced technologies to space-based services. Start-ups work with mentors to sharpen objectives, prioritize time and resources, raise capital, build networks and engage with experts working on the frontiers of research.
Similarly, the CDL health stream helps seed-stage teams bring human health innovations to market. This stream is focused on improving the quality, speed, cost and accessibility of healthcare delivery and improving the operational efficiency of the health system.
National Aeronautics and Space Administration
The United States has the largest and most comprehensive space program in the world. The National Aeronautics and Space Administration's (NASA) proposed budget for is $24.8 billion, an increase of almost 7% above its current funding. NASA's deep-space exploration, science missions, space technology and STEM outreach programs are the biggest beneficiaries of this proposed increase in funding.
CSA and NASA have a long history of successful partnerships that spans space activities in all areas, including space exploration, Earth observation, science, technology, education and outreach, as well as international policy development. The mutual trust in our capabilities that has been built through this relationship is evident in the integration of Canadian astronauts within the U.S. Corps of Astronauts in Houston, and the integration of the ISS robotic operations between CSA and NASA teams.
As part of the upcoming Lunar Gateway program, CSA and the Canadian space sector are working to provide NASA and partners with Canadarm3—the most sophisticated space robotics system ever developed. The first Artemis crewed mission around the Moon, scheduled for , will be a milestone deep-space mission and will include a Canadian astronaut as one of its four crewmembers.
Appendix H Transferring Medical Technologies Across Remote Environments
In the coming decades, the nature of healthcare delivery in space will change markedly. As astronauts venture farther into the solar system, ground-based oversight of onboard medical care will become more limited by reason of the astronomical distances between Earth and the crew. In particular, medical evacuation from deep space of a seriously ill astronaut for emergency care on Earth will no longer be an option.
Accordingly, crew medical facilities aboard spacecraft must be redesigned to augment the autonomy of deep-space astronauts and to support a broader range of medical and surgical eventualities. Future facilities will incorporate patient-centric, point-of-care and virtual care modalities. Intelligent onboard systems will be integrated to aid the crew medical officer with health monitoring, diagnosis and therapy.
The following graphic depicts a few essential technologies that will become elements of next-generation crew medical systems.

Deep-Space Healthcare System - Text version
- Non-invasive vital-signs monitoring, with AI-enabled, real-time screening of relevant data
- Polyvalent and light-weight medical imaging, such as AI-assisted ultrasonography
- Medical knowledge database with clinical decision support
- In-space 3-D medical device manufacturing
- Procedural training / simulation and support with 3-D, augmented-reality visualization
- Canada-based medical operations control centre, with a broad network of available consultants for telemedicine support
- Integrated and automated crew-health maintenance and injury-prevention program
- Compact point-of-care biological sample analyzer ("
lab-on-a-chip
")
Remote regions on Earth, however, are similarly expansive, austere and isolated. Working conditions of physicians and nurses in northern Canada where access to clinical specialists, biomedical engineers and leading-edge technologies is limited can be as challenging as in space. Could approaches and methodologies developed for future astronauts also bring benefit to the management of healthcare on Earth? Could training and advanced support developed for deep space also empower practitioners working in rural and remote settings?
The following series of clinical vignettes provides a glimpse into potential terrestrial applications of novel technologies developed for deep space.
Point-of-Care Analyzer
- A crew medical officer on a spacecraft in transit to Mars reviews results of a routine blood biomarker survey from the entire crew as a screen for cancerous mutations following exposure to the radiation environment of deep space.
- A nurse practitioner managing a rural walk-in clinic examines results of a blood sample analysis of infection markers from a middle-aged patient being treating locally for an upper urinary tract infection, rather than referring the man to the regional hospital.
Remote Telemedicine
- A crew medical officer at a lunar outpost is tele-mentored (receives verbal guidance) from a medical specialist on Earth and visually via her heads-up display to perform a chest-tube insertion on a crew member who suffered a collapsed lung in a decompression incident.
- An emergency physician in a northern community is guided through a burr-hole procedure for a traumatic brain bleed, using the same technology.
Crew Health Maintenance & Injury Prevention
- An AI-enabled system autonomously tracks the onboard crew's exercise, food & fluid intake, sleep patterns, light and sound exposure, then offers tailored suggestions to optimize their health and performance.
- An elderly woman lives independently with an intelligent home monitoring system that enables her safe mobility through fall-prevention sensors.
Clinical Decision Support
- A crew medical officer at the Mars Base takes photographs of a rash that another astronaut has developed, feeds them into the AI-enabled clinical assistant and obtains a diagnosis with suggested treatment.
- A community physician doing rounds among critically ill patients uses his portable AI clinical assistant to help make sense of a patient's complex set of vital signs and laboratory results.
Training / Simulation
- A crew medical officer aboard a Mars transfer vehicle uses a heads-up display with augmented reality overlay to review the technique to anesthetize and suture the eyebrow of a fellow crew member who suffered a laceration.
- A family physician in his office uses the same system to review the anatomy and procedural technique before doing a joint infiltration in a patient with osteoarthritic pain.
Non-Invasive Vital Signs Monitoring
- While working on an experiment inside the Lunar Gateway, the crew medical officer receives an alarm in his earbud about subtle signs of an abnormal heart rhythm developing in a crew member who is performing a spacewalk.
- A community nurse in the Arctic receives an alarm on her smartphone of early signs of respiratory distress in a village elder with chronic obstructive pulmonary disease.
Imaging
- While in transit from Earth to Mars, renal ultrasounds are regularly performed on all crew members for the early detection of kidney stones, using an AI-enabled system that provides on-the-fly corrective feedback on the probe's position to the operator.
- A rural midwife performs a regular pregnancy follow-up ultrasound using the same system.
These are just a few examples of technologies that could be transferred across practice locales. Since the needs of healthcare delivery in deep space and remote regions are comparable, it can be expected that the solutions are also similar. Lessons learned from deep space can be adapted to bring benefit to Indigenous and underserved populations or to chronic care patients who are being monitored remotely from their homes. These innovations could be transformative for national healthcare, leading to lower costs and better health outcomes.